Lung cancer is one of the most common cancers in the UK. Around 48,000 people are diagnosed with lung cancer each year, accounting for around 13% of all new cancer cases.
Cancers of the lung can originate in the lungs or can spread to the lungs from another part of the body. The former is known as primary lung cancer, while the latter is called secondary lung cancer. This page will focus on primary lung cancer.
What is lung cancer?
Like all other types of cancer, lung cancer happens when certain cells can no longer be controlled by your body and start to change and become abnormal. The number of abnormal cells starts to increase and multiply out of control.
Over time, these can form a lump called a tumour. However, it is also possible for cancerous cells to be present in your body and not cause a noticeable tumour.
Unfortunately, lung cancer is also one of the most common causes of cancer death in the UK, with around 95 people every day dying from the disease. However, lung cancer mortality rates are predicted to fall over the coming years as earlier diagnoses and new treatments improve patient outcomes.
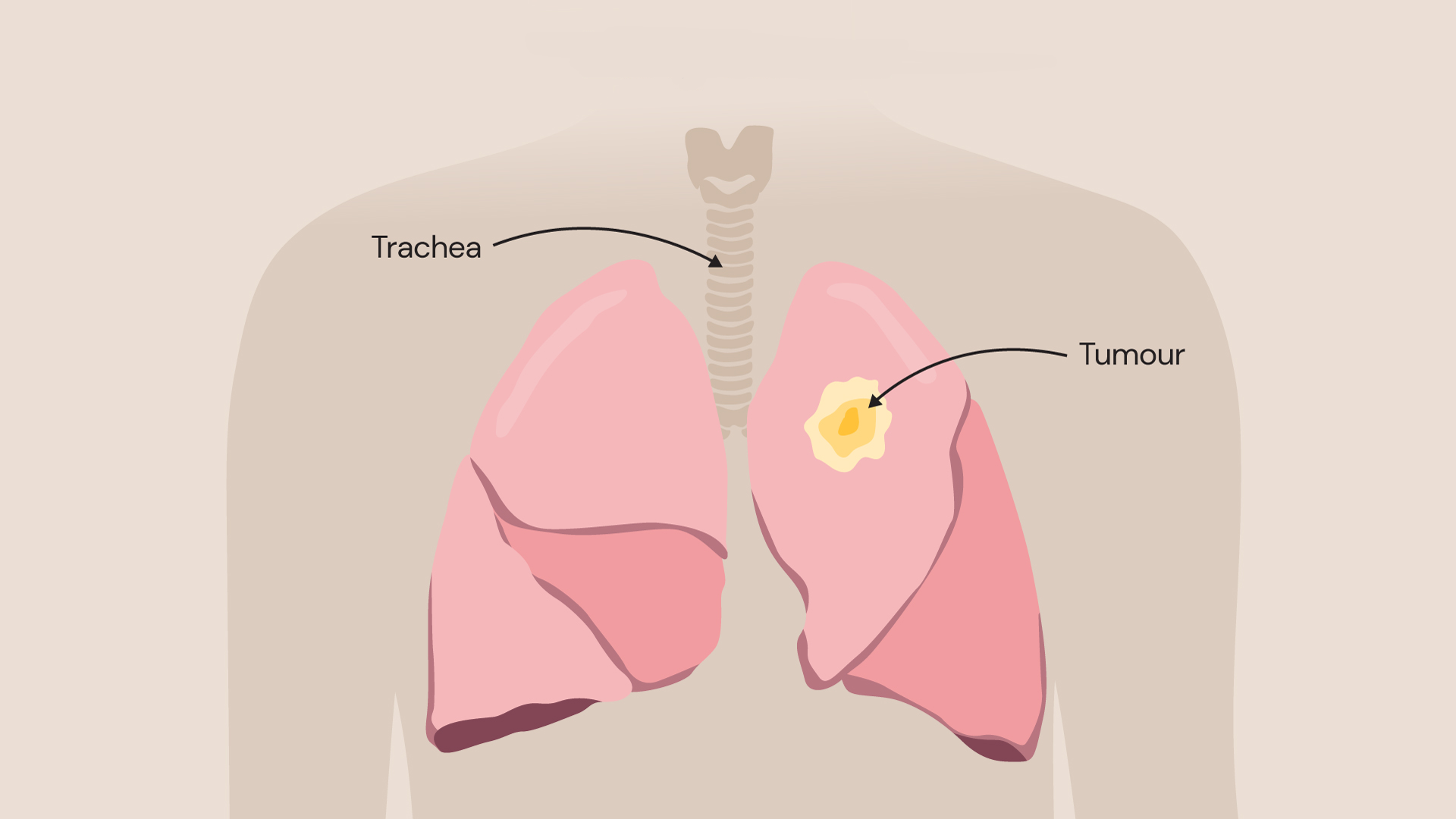
Over time, a lump called a tumour can develop in your lungs.
Types of lung cancer
There are two main types of primary lung cancer. Each type is determined by the type of cell that the cancer first started growing in.
Non-small cell lung cancer
This is the most common form of primary lung cancer, being diagnosed in around 80-85% of cases. There are three different types of non-small-cell lung cancer:
- Squamous cell carcinoma: This usually begins in the passages that bring air into the lungs. It also grows more slowly than other types of lung cancer.
- Adenocarcinoma: This is the most common type of non-small cell lung cancer and starts in the glands that line your airways.
- Large-cell carcinoma: This type can appear in any part of the lung and tends to grow and spread quickly.
Small-cell lung cancer
A much rarer form of primary lung cancer, small-cell lung cancer is usually more aggressive and spreads faster.
What causes lung cancer?
It is well known that most cases of lung cancer are due to smoking. However, there is evidence that small dust-like particles in air pollution are also linked. How these particles damage DNA in cells to cause cancer is not fully understood, but the smallest particles known as PM10 and PM2.5 are known to be associated.
Exposures to chemicals and substances in the workplace may also contribute to an increased risk. These include asbestos which you may be exposed to during building work; silica during glass making or bricklaying; as well as regular exposure to diesel exhaust fumes such as that experienced by professional mechanics and drivers.
Lung cancer is strongly linked to age with disease rates increasing sharply after 45.
Lung cancer symptoms
There are not usually any signs of lung cancer in the initial stages of the condition. However, as the cancer progresses, you may start to develop symptoms including:
- a persistent cough
- coughing up blood
- ongoing chest infections
- persistent breathlessness
- unexplained tiredness
- unexplained weight loss
- chest or shoulder pain
- aching or pain when breathing or coughing
If you notice any of these symptoms, you should make an appointment with your doctor.
How is lung cancer diagnosed?
Royal Brompton and Harefield hospitals are world-leading centres for heart and lung care. We diagnose and treat hundreds of patients with lung cancer each year, with many coming from abroad just to see our consultants privately.
We have internationally renowned experts in imaging and histopathology who can diagnose the type, location, and stage of lung cancer with the greatest precision. This helps guide procedures to remove lung cancer while avoiding harming healthy lung tissues.
Any lung cancer diagnosis starts with a consultation where you will discuss your symptoms and concerns with your chosen consultant.
You will be asked about your lifestyle and your medical history so that we can build a picture of your day-to-day life. You may also be asked to breathe into a device called a spirometer which measures how much air you breathe in and out.
If your doctor suspects you may have lung cancer, you will be referred for several tests to determine if you have it, and if you do, what type you have and if it has spread. These tests may include:
- a blood test to rule out infections or other causes of your symptoms
- a chest x-ray which will provide a picture of what is happening inside your lungs, enabling us to detect any masses which may or may not be cancerous
- a CT scan – usually performed following a chest x-ray, a CT scan provides a detailed image of your lungs so that any abnormalities can be seen more clearly
- a PET-CT scan – a different type of imaging test which may be done if your CT scan suggests that you have cancer. A PET-CT scan shows the position of active cells and helps your respiratory consultant decide which investigations/treatments would be best for you
- a lung cancer biopsy – a procedure used to take a small sample of tissue, which can then be looked at under a microscope to get more information about the cells, including if they are cancerous and if they are, the type and stage cancer you have
If you need a lung cancer biopsy, this may be carried out in a few different ways. You may have:
- a bronchoscopy (in which a thin tube is inserted through the mouth or the nose). Our experts use the latest Ion robot-assisted lung cancer biopsy technology to sample tumours when they are still very small in size for a better chance of treatment success
- percutaneous needle biopsy (where a needle is placed directly through the skin into the lungs). Audits of our service demonstrate 95.3% diagnostic accuracy with 78% same-day discharge rates.
- thoracoscopy or mediastinoscopy (in which tubes with cameras are inserted into the chest through surgical incisions).
Your lung care specialist will explain which tests you need and what you can expect to happen.
Our consultant thoracic surgeon, Professor Eric Lim, explains the importance of early lung cancer diagnosis.
Lung cancer risk assessment service
Unfortunately, lung cancer is difficult to treat when it is diagnosed at an advanced stage, with only 1 in 5 people surviving. It is therefore important that the disease is captured in its earliest stages for the greatest chance of treatment success.
Our lung cancer risk assessment service is available for people that are at an increased risk of developing the condition, offering them a chance to be comprehensively reviewed by one of our respiratory consultants.
People that are at an increased risk of developing lung cancer include those who:
- regularly smoke or have a history of heavy smoking
- have a strong family history of lung cancer
- are over 50 years of age (8 in 10 cases of lung cancer occur in people over 60, but it can occur at younger ages too)
Our specialists will assess your risk of lung cancer during a consultation and recommend further testing if necessary.
Lung cancer treatment
Our respiratory consultants at Royal Brompton and Harefield hospitals are experts in lung cancer care. They are pioneers in minimally invasive lung cancer surgical and non-surgical procedures and are internationally renowned in this field.
We work closely with cancer specialists at Royal Marsden Hospital in London, a world-renowned cancer centre, and Mount Vernon Cancer Centre in Northwood. Consultants at both hospitals provide expertise in chemotherapy, radiotherapy, and immunotherapy, while our specialists provide surgical and non-surgical procedures for lung cancer.
The treatment recommended for your lung cancer will depend on the type you have, how large the cancer is and how far it has spread. Explore our lung cancer treatments below.
Lung tumour ablation
Lung tumour ablation is a minimally invasive technique that avoids the need for surgery. It uses either hot or freezing temperatures applied directly to the tumour to kill the cancer cells, while avoiding harm to surrounding healthy lung tissues.
Tumour ablation may be recommended if:
- surgery is not an option for you
- there are only a few small tumours in your lungs (both primary and secondary tumours can be treated using this method)
- the tumour is in a location in the lungs where it is difficult to operate
Tumour ablation can be applied in two ways, depending on the location of the tumour.
Endobronchial tumour ablation (endobronchial cryotherapy)
If the lung tumour is in the airways, a procedure called endobronchial cryotherapy may be performed where a bronchoscope (a tube-like device with a camera at its end) is used to reach it.
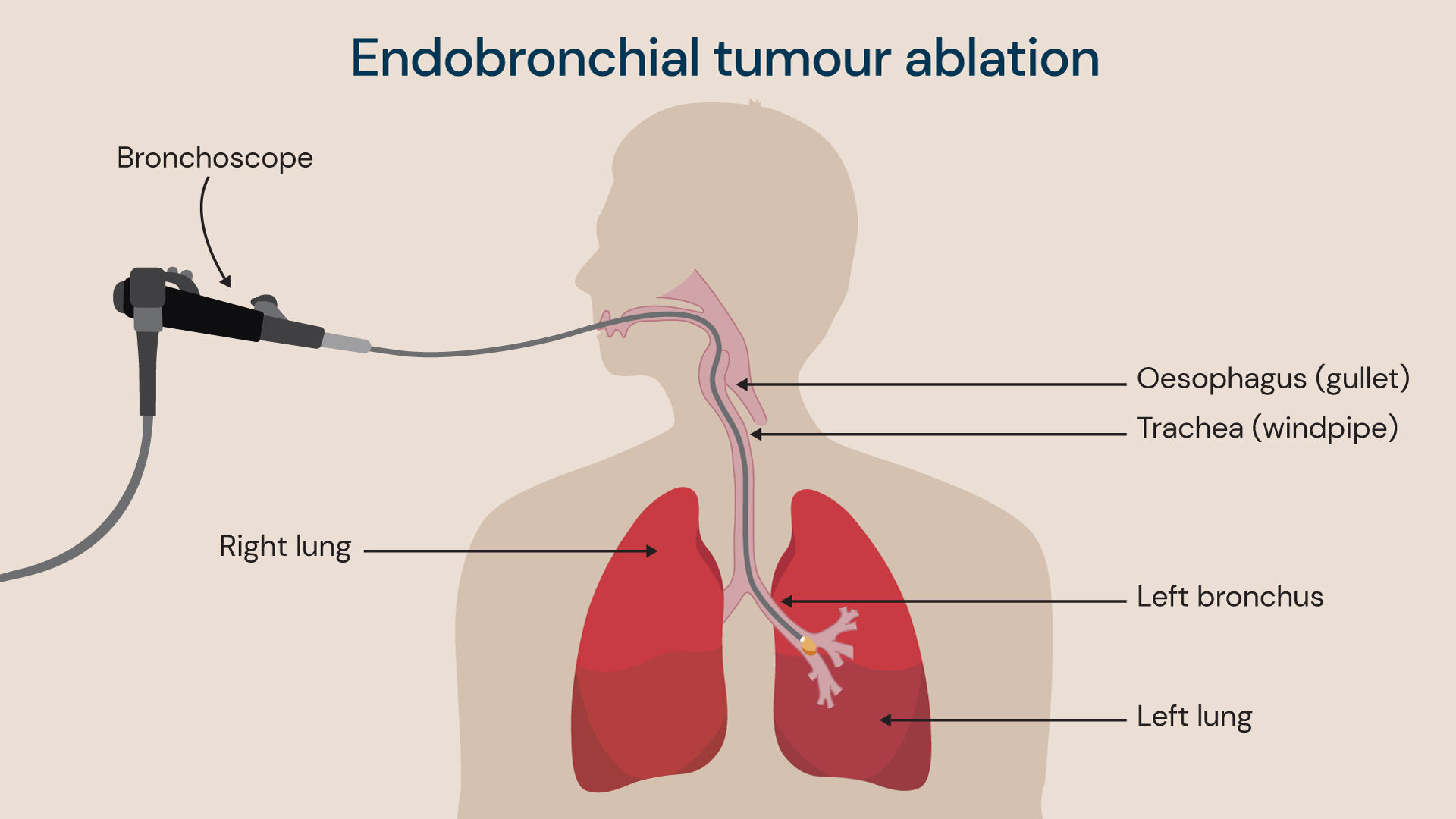
Endobronchial cryotherapy: A bronchoscope is used to reach the lung tumour in the airways, before applying very cold temperatures to freeze and kill it.
Our consultants apply a cryogen (a substance that produces very cold temperatures between -78C and -187C) from the tip of the bronchoscope to freeze and kill the cancer cells.
This procedure takes approximately 20 minutes to complete, and the patient is sedated with general anaesthetic. This treatment is offered at Royal Brompton Hospital but is not available at Harefield Hospital.
Percutaneous tumour ablation
Percutaneous means ‘through the skin’. Our consultants use an innovative ‘pinhole’ technique for our percutaneous tumour ablation procedures where a needle-like probe is inserted into the lungs via the skin and is guided to the site of the tumour with medical imaging to deliver treatment.
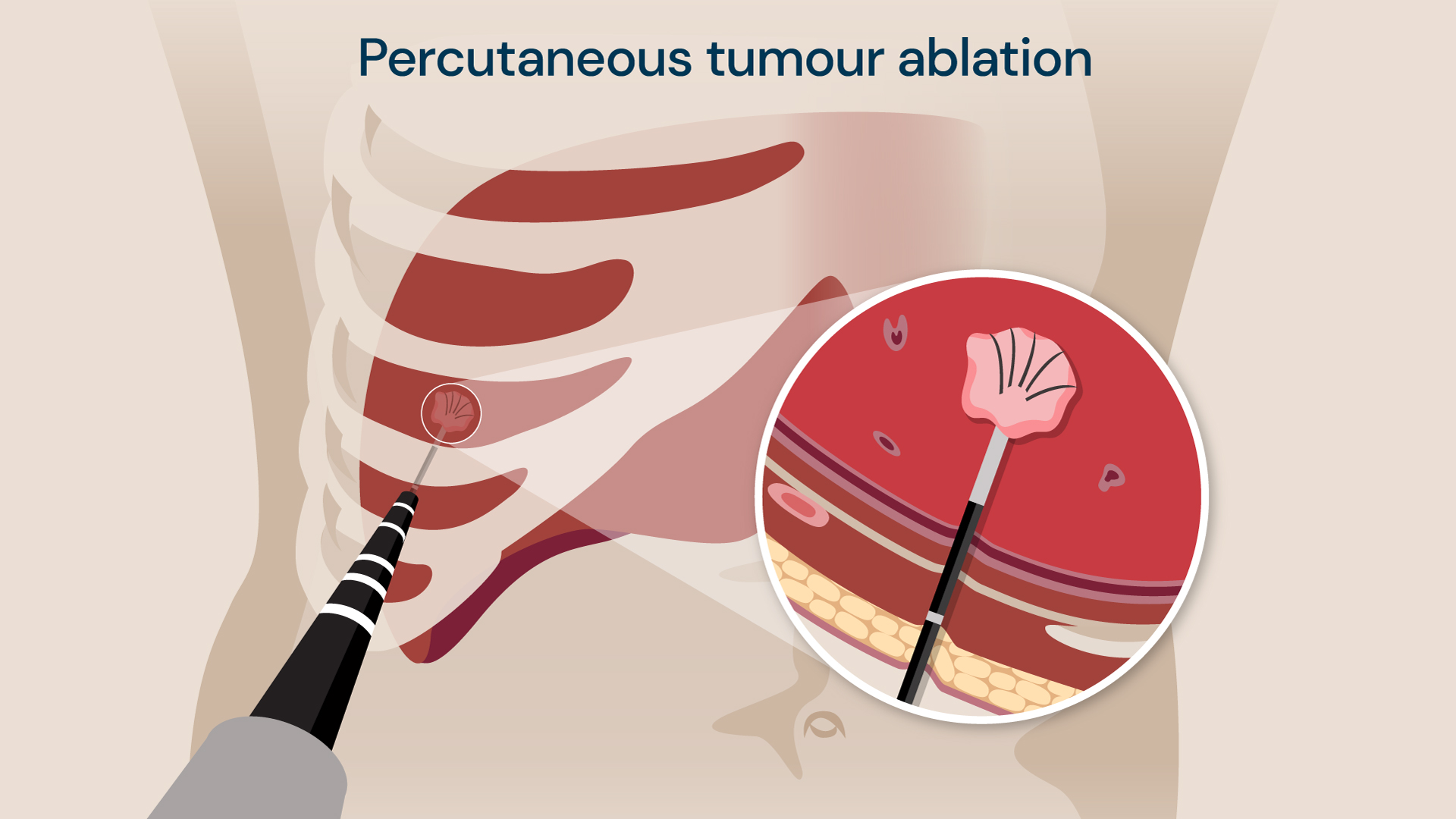
A ‘pinhole’ technique is used by our consultants to deliver hot or freezing treatment to kill the cancer cells in the lung.
Hot (microwave therapy) or freezing (cryotherapy) temperatures are used at the tip of the probe to kill the tumour cells. This procedure is used when the tumour is located outside the airway.
Hot temperatures may be used in deeper lung tissues (where there is a lot of lung tissue surrounding the tumour), while cold temperatures may be used near the delicate outer lining of the lung. This procedure is usually performed with general anaesthetic and takes 1 hour.
We are pleased with our local tumour control rate of 93.1%, with 99.1% of patients experiencing minor or no complications. The local tumour control rate means that cancer has not returned at the site of treatment.
Awake ablation
Our consultants have developed a new technique called ‘awake ablation’ where local anaesthetic is used. The specific area to be treated is numbed rather than the patient being sedated. This is useful for patients that cannot receive general anaesthetic.
Our awake ablation technique has won the coveted LaingBuisson award in 2022 for improving healthcare outcomes, as it offers patients an option to remove their lung tumour with a minimally invasive technique when this was not previously possible.
Single-port video-assisted thoracoscopic surgery (VATS)
For larger lung tumours, surgery may be needed to remove the part of the lung affected.
This is traditionally performed with an open-chest surgery, where the breastbone is cut to access the tumour. However, not all patients are suitable for this procedure, such as if they have other health concerns that make them high risk.
Our consultant thoracic surgeons offer a keyhole surgical procedure to remove lung cancer, called single-port video-assisted thoracoscopic surgery (VATS). This can be offered to patients as a minimally invasive alternative to open chest surgery.
A single incision is made in between the ribs (a port) to enable our surgeons to insert a camera and surgical instruments needed for the VATS procedure.
Our consultants were actively involved in the VIOLET study to understand the outcomes of the VATS procedure. The study showed that the VATS procedure resulted in significantly less pain, fewer complications and a faster recovery when compared to open chest surgery.
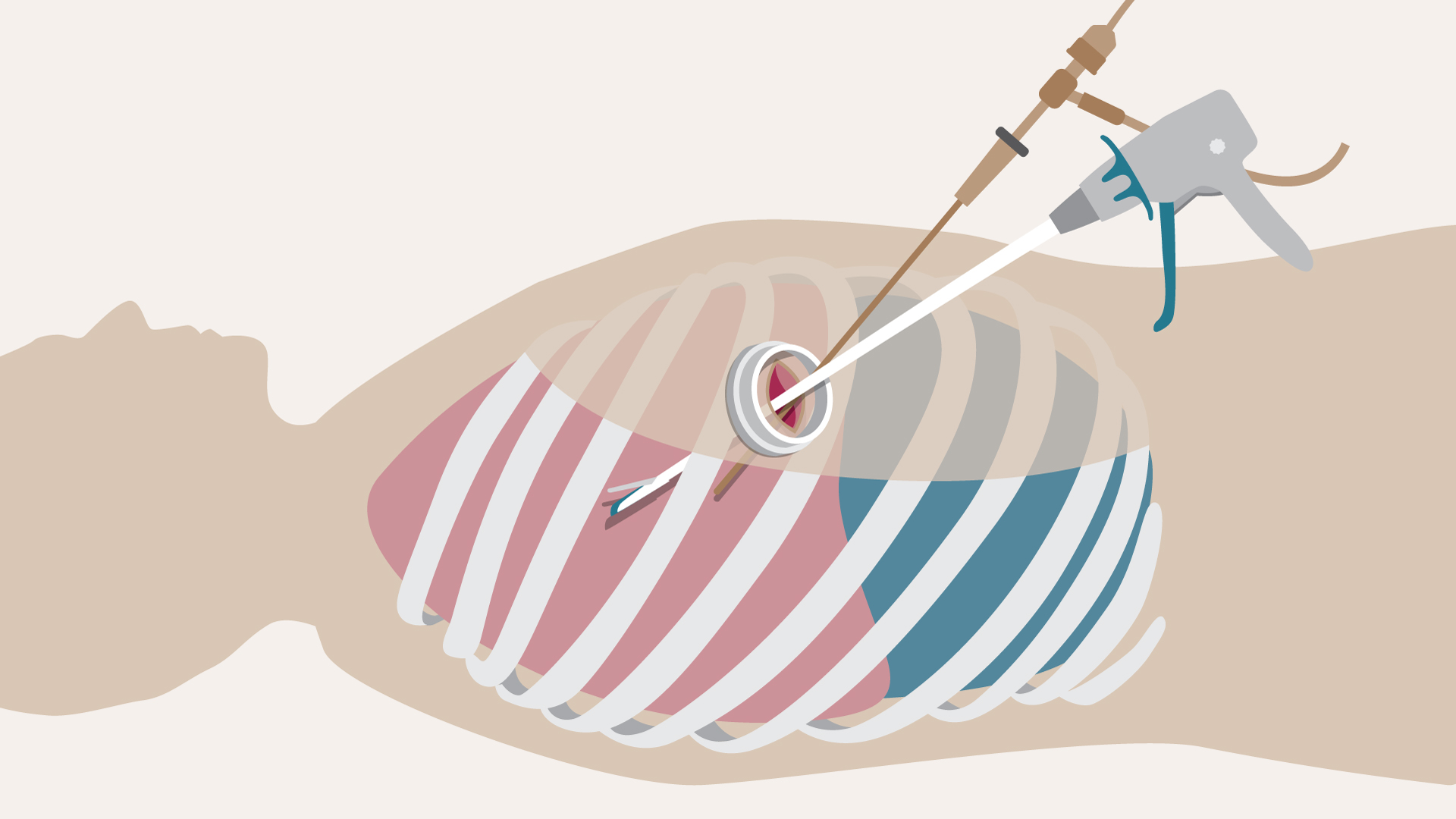
The VATS procedure.
Cryotherapy pain relief for chest surgery
The recovery process following open chest surgery and minimally invasive VATS procedures is associated with pain that needs to be managed with medication. Patients can also experience limited movement due to pain that requires physiotherapy to support healing.
Royal Brompton Hospital is the first in the UK to offer cryotherapy treatment that is applied during chest surgery to offer pain relief for up to 6 months post-surgery. It works by temporarily ‘shutting off’ the affected nerves in the chest that transmit pain signals to the brain, numbing the area operated on.
Related services
-
CT scan
A CT uses X-rays and a computer to produce images of many structures inside the body.
-
Diagnostic tests for lung conditions
Our advanced, high-quality diagnostic facilities can help rapidly diagnose lung conditions.
-
Hypoxic challenge test
A hypoxic challenge test is used to assess whether you need extra oxygen while travelling on a plane, due to the reduced levels of oxygen in aircraft cabins.
-
Lung cancer risk assessment
Our world-leading specialists can assess your risk of developing lung cancer during a consultation.
-
Lung health assessment
Our lung health assessment service is accessible to patients with a range of symptoms, including breathlessness, cough, chest pain, and wheezing.
-
MRI scan
An MRI scan is a medical imaging technique that uses a magnetic field and radio waves to create pictures of an internal cross-section of the body’s structures.
-
Percutaneous cryotherapy
Percutaneous cryotherapy treatment involves freezing a lung tumour – to kill the cells in it – using a CT scanner for guidance.
-
Tumour ablation for lung cancer
Tumour ablation is a procedure that uses heat or cold treatment to kill a tumour inside the lungs. Find out more about this procedure.
Locations
Diagnosis and treatment for lung cancer is available at the following locations: