Fungal spores in the air we breathe can cause a variety of health problems. They can make symptoms of asthma more severe and for people with weakened immune systems, can lead to life-threatening symptoms. Our experts can help accurately diagnose fungal lung disease to ensure patients receive the best care.
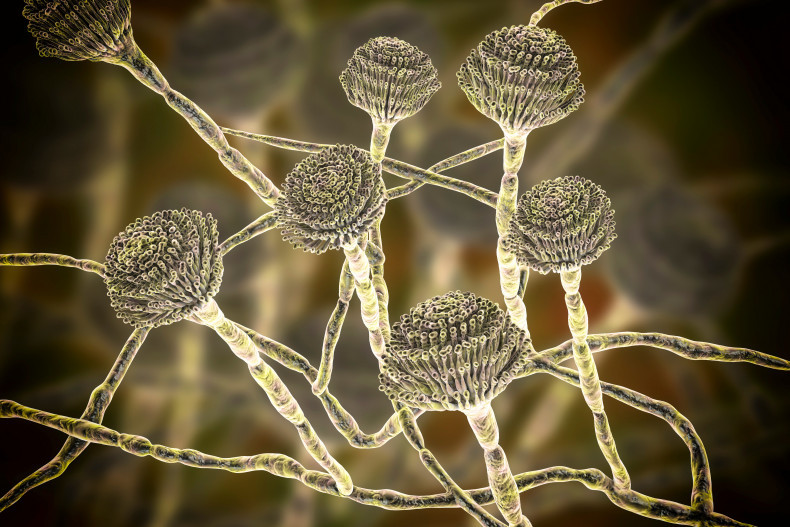
A 3D illustration of the fungus Aspergillus
What is a fungus?
You will probably be most familiar with the types of fungus (plural fungi) in your shopping basket, as they include yeast used for bread-making and mushrooms used for cooking.
However, they come in all shapes and sizes and the smallest microscopic types can lead to health problems. These include thrush that is a common mild genital skin infection, but also fungal nail infections and athlete’s foot.
Sometimes, fungal health problems can become more serious, particularly if they affect the lungs.
How do fungi cause disease in the lungs?
We are always breathing in microscopic pieces of fungi called spores, which enable them to multiply and spread inside our lungs. Thankfully, this rarely causes disease in healthy people as our immune system usually gets rid of them.
When fungi cause disease in the lungs, they do so in two ways. The first way is by fungal spores causing irritation and inflammation of your airways (usually in those with asthma) and the second is by directly infecting your lungs (usually in those with a weakened immune system).
We cover both types of fungal disease in more detail below.
Asthma and sensitivity to fungi
Sensitivity to fungi can make symptoms of asthma worse – it is estimated that up to 50% of adults with asthma that are referred to a specialist are sensitive to one or more types of fungi that cause disease.
This has led to doctors defining a new type of asthma, called ‘severe asthma with fungal sensitisation’ (SAFS).
If a patient has severe asthma that cannot be controlled with conventional treatments, they are recommended to do a blood test which helps doctors understand whether they have a sensitivity to fungi. If they do, they may have SAFS. Your doctor may also conduct a skin prick allergy test if they feel it is needed to determine sensitivity to fungi.
‘Allergic bronchopulmonary aspergillosis’ (ABPA) is another condition that affects 1% of patients with asthma. Like SAFS, it can make asthma more severe, but the sensitivity is specific to a type of fungi called aspergillus. ABPA can result in dilatation of your airways, recurrent infection and flares of your asthma.
Recent studies have shown promising results in treating both conditions with antifungal treatments to better ease their symptoms and help them breathe better.
“If a patient is experiencing severe asthma symptoms that are not being eased with asthma medications, we recommend they contact their doctor to explore whether their lungs may be sensitive to fungi. This can help their doctor provide the best treatment for them,” explains our consultant respiratory physician, Dr Anand Shah.

A skin prick allergy test
Who can get a fungal lung infection?
The main type of fungal lung infection in the UK is called aspergillosis and like ABPA is caused by the aspergillus fungus.
It rarely affects healthy people but can cause severe disease in those with health conditions that weaken their immune system (such as cystic fibrosis) or people who take medications that suppress their immune system (such as patients with cancer or rheumatoid arthritis).
Patients can experience aspergillosis in different ways depending on how the infection spreads and the other health problems they have.
Sometimes, patients can develop a cavity in their lungs, which is a large abnormal air-filled space. The cavity is formed by other lung infections such as tuberculosis and lung conditions including COPD and sarcoidosis.
The fungal infection can form a large ball called an ‘aspergilloma’ in this lung cavity which can result in complications, such as coughing up blood that can be life-threatening.
In patients with severely weakened immune systems, such as those undergoing a bone marrow transplant or receiving chemotherapy for cancer, they can be at risk of ‘invasive aspergillosis’.
Invasive aspergillosis is a serious form of the disease which can spread from the lungs to other parts of the body, including the brain.
“It can be difficult for your doctor to diagnose an aspergilloma or invasive aspergillosis, as the symptoms of fever, cough and shortness of breath are not specific to the conditions. At Royal Brompton and Harefield hospitals, we have expertise in the imaging and treatment of fungal lung diseases to ensure we capture infections sooner,” explains our infectious diseases physician, Professor Darius Armstrong-James.

Young patients with cystic fibrosis are at risk of aspergillosis
Monitoring for resistance to antifungal treatments
The first-line antifungal treatments for aspergillosis belong to a group of drugs called ‘triazoles’.
Unfortunately, a growing number of patients have infections that are resistant to these drugs, which greatly influences treatment outcomes.
Resistance can arise in two main ways. The first way is spontaneously during long-term therapy with these drugs as in the case of chronic aspergillosis.
The second way is through the agriculture industry as similar antifungal treatments are used to prevent fungi damaging crops (they are used as pesticides). These aspergillus strains that acquire antifungal resistance in the environment are then breathed in and infect people that are susceptible.
A recent study showed that patients with aspergillosis that was resistant to a certain triazole drug were up to 30% more likely to die from the infection. Fortunately, alternative antifungal treatments are available that are also effective.
“Drug sensitivity testing and ongoing therapeutic drug monitoring are an important part of treating aspergillosis to identify resistance as soon as possible and ensure the best outcomes – particularly in those receiving long-term antifungal therapy,” explains Dr Shah.
Multi-disciplinary expertise needed for accurate diagnosis
“Royal Brompton and Harefield hospitals is the largest centre for fungal lung diseases in south England and we see over 600 patients a year. Our multi-disciplinary expertise enables us to quickly and accurately diagnose these conditions which can otherwise be challenging and require specialist diagnostic tools,” explains Dr Shah.
Professor Armstrong-James adds: “Our lung imaging consultants can help identify even the most subtle signs of fungal lung disease and work alongside our diagnostic experts to detect infectious diseases not often seen at other centres.
“Our combined expertise enables us to detect antifungal resistance at the earliest stages to deliver an optimal treatment plan tailored to each patient. We also have some of the world’s leading cardiothoracic surgeons should surgery be required, as may be the case for an aspergilloma.”
Related content
-
Fungal lung diseases
Some fungi can affect the lungs and if left untreated can cause serious lung diseases, including severe cases of asthma. Learn more.
-
Respiratory medicine
Our respiratory medicine services at Royal Brompton and Harefield hospitals are world-renowned for their innovative and ground-breaking treatments and patient care.
-
Children's respiratory medicine
Our world-class respiratory service cares for children affected by breathing difficulties such as asthma, lung infections and sleep disordered breathing.
-
Chronic lung infection
Chronic lung infections may be persistent, but they can be treated. Discover how we can accurately diagnose and treat chronic lung infections.
-
Lung health assessment
Our lung health assessment service is accessible to patients with a range of symptoms, including breathlessness, cough, chest pain, and wheezing.

