Sarcoidosis is a rare disease, affecting around 1 in every 10,000 people. Every year in the UK about 3,000 to 4,000 people are diagnosed with the condition. Sarcoidosis typically affects young adult individuals between 25 and 60 years of age. Both genders can be equally affected, but there is a second peak of prevalence in women above 55 years old.
What is sarcoidosis?
Sarcoidosis is a rare inflammatory condition that develops when your immune system overreacts, causing areas of excessive inflammation to develop. You may be genetically predisposed to develop such a reaction to environmental (organic and non-organic) triggers.
Your immune system is an important part of your body, helping to protect you against germs and illnesses. The immune system can recognise and destroy potentially dangerous germs. Furthermore, it should terminate the response quickly once the threat has been eliminated. However, sometimes it may malfunction and create inflammation that gets out of control in patients with sarcoidosis.
Sarcoidosis occurs when a specific inflammation causes tiny lumps, called granulomas, to develop on the body’s tissues. Granulomas can develop anywhere on the body, but they most often form in the lungs, skin, and lymph glands. Between 90 and 95% of patients with sarcoidosis are affected in the lungs, known as pulmonary sarcoidosis.
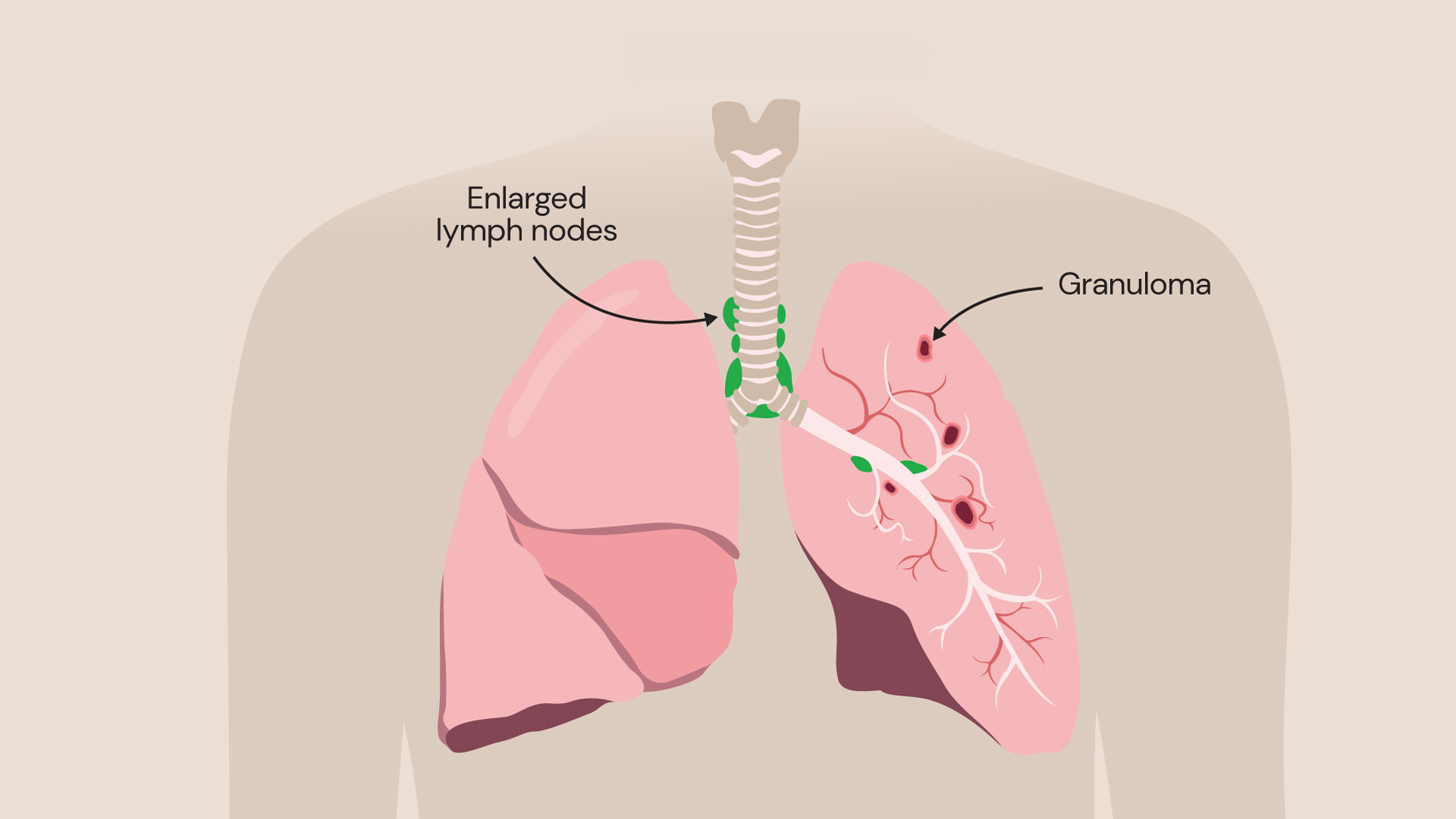
Sarcoidosis occurs when granulomas develop on the body's tissues, such as in the lungs.
For most people, sarcoidosis is a mild disease and is rarely severe or life-threatening. Granulomas will heal and disappear on their own without treatment.
However, if they do not heal, scarring may develop inside the lungs and affect the way that you breathe. This is known as pulmonary fibrosis, and while it is quite rare, it can cause further complications with your health.
Sarcoidosis symptoms
Most people with sarcoidosis rarely experience any symptoms of the condition and the fact that plenty of granulomas heal and go away on their own means that many people may have had sarcoidosis without even knowing it.
Nevertheless, some people with pulmonary sarcoidosis will experience symptoms, which could include:
- shortness of breath that may get worse with activity
- a dry, persistent cough
- chest pain
- wheezing
- reduction in the amount of air in your lungs
It is important to be aware that not all the symptoms associated with sarcoidosis relate directly to your lungs and breathing. Cardiac involvement and/or complications are associated with high morbidity and mortality in sarcoidosis.
In that case, patients may experience prominent palpitations (irregular or fast heartbeat), chest pain (angina or nonspecific), dizzy spells, light headiness or even loss of consciousness. Heart rhythm disturbances can be identified by an electrocardiogram (ECG) and holter monitoring.
A detailed cardio-respiratory workup is usually performed for patients with suspected cardiac sarcoidosis.
Lots of people with the condition also experience other effects that affect their quality of life and relate more closely to an overactive immune system. These include:
- extreme tiredness
- weight loss
- fever
- night sweats
- pain in their bones and joints
- skin rashes
- swollen lymph nodes
As the symptoms of sarcoidosis may also indicate other health conditions, it is important to speak to your doctor to discuss what is happening and to get a diagnosis.
What is also important to know is that sarcoidosis tends to remain in the same place in each person diagnosed with it. It rarely moves from organ to organ, so if you have sarcoidosis only in your lungs at the time of diagnosis, it is unlikely to occur in another part of your body too.
What causes sarcoidosis?
We do not know why some people develop sarcoidosis and other people do not.
Sarcoidosis can affect people of any age too, although it is most often diagnosed in people in early to middle adulthood.
Some experts think that the condition is usually triggered by an event such as a severe infection that sends your immune system into overdrive. However, this trigger could be different in each person with sarcoidosis.
Some people also think that sarcoidosis may be hereditary, so if you have a family member with the condition, you may be more likely to develop it too.
How is sarcoidosis diagnosed?
A diagnosis of sarcoidosis starts with your complete medical history and a conversation about the symptoms that you are experiencing. A biopsy may often be required to confirm the diagnosis histologically.
You may also need to have a range of different tests, including:
- blood tests. Blood tests can assess the function of your organs and tell whether you have an infection or another underlying health condition
- chest X-ray. A chest X-ray looks at the size, shape and location of the lungs and lung structures, including any abnormalities such as areas of inflammation and granulomas. However, even if your chest X-ray shows that you have had sarcoidosis previously, it may not have any long-term effect on your quality of life
- CT scan. A more advanced imaging test, a CT scan shows your lungs in greater detail and can be used to detect evidence of granulomas in the lungs, monitor disease progression and more
- pulmonary function test. This test measures how much air moves in and out of your lungs
- bronchoscopy. This test uses a long, thin tube with a light and camera at the end that is passed down through your airway into your lungs, enabling a live view of the lungs and bronchi, which are the main airways of the lungs. A biopsy (tissue sample) can also be taken at this time if needed
- FDG-PET scan. This can offer an assessment of inflammation in your whole body and identify sites that could be biopsied to offer a confident diagnosis
- cardiac tests for cardiac sarcoidosis
- neurological workup including brain and spinal MRI, lumbar puncture, nerve conduction studies and EEG depending on the patient’s symptoms
Treatment for sarcoidosis
Most people with sarcoidosis do not need any treatment at all, as most granulomas go away on their own within several months or years. However, you may want to consider taking over-the-counter pain medications such as paracetamol or ibuprofen to relieve any symptoms that you might be experiencing, like joint pain or discomfort. In the meantime, you will be closely monitored to see how your condition is progressing.
Steroids for sarcoidosis
If you do need treatment for sarcoidosis, you will initially be prescribed steroid medication.
Steroids work by reducing inflammation, which can relieve some of your symptoms and prevent scarring. Nevertheless, just like any other medication, there are side effects associated with taking steroid medication. Side effects vary depending on the dose and duration of your treatment.
Short-term side effects of steroid use include:
- increased appetite
- weight gain
- indigestion and heartburn
- difficulty sleeping
- mood swings and irritability
However, long-term steroid use can result in side effects like:
- raised blood sugar levels, especially if you have a family history of diabetes
- weakened bones, resulting in a condition called osteoporosis
- high blood pressure
- eye problems, including cataracts or glaucoma
Immunotherapy
If steroid creams are not proving to be effective at reducing your symptoms, you may be offered immunotherapy.
This is a treatment that targets your immune system, calming it down to reduce the formation of more granulomas and ease your symptoms.
Our expert lung care team will talk to you about the different options for treating pulmonary sarcoidosis and create a bespoke treatment plan to meet your needs.
Other treatments
In severe cases of lung fibrosis (scarring), a patient may require oxygen therapy or lung transplantation.
More unusually, in cases of heart failure, an implantable cardioverter defibrillator may need to be fitted which helps regulate your heart’s rhythm.
Locations
Our specialists can treat sarcoidosis at the following locations:
Discover our respiratory medicine experts
Meet our team of leading respiratory medicine specialists. From lung health to advanced interventions, our experts are here to provide personalised care tailored to your respiratory needs.
