What is myocarditis?
Myocarditis is inflammation of the heart muscle (myocardium), which reduces its ability to pump blood. Government figures in the UK show that in 2017 there were 2,000 hospital admissions for myocarditis.
The condition causes symptoms such as shortness of breath, chest pain and irregular heart rhythms (arrhythmias). Most people recover from myocarditis without complications, but in rare cases, it can cause damage to the heart.
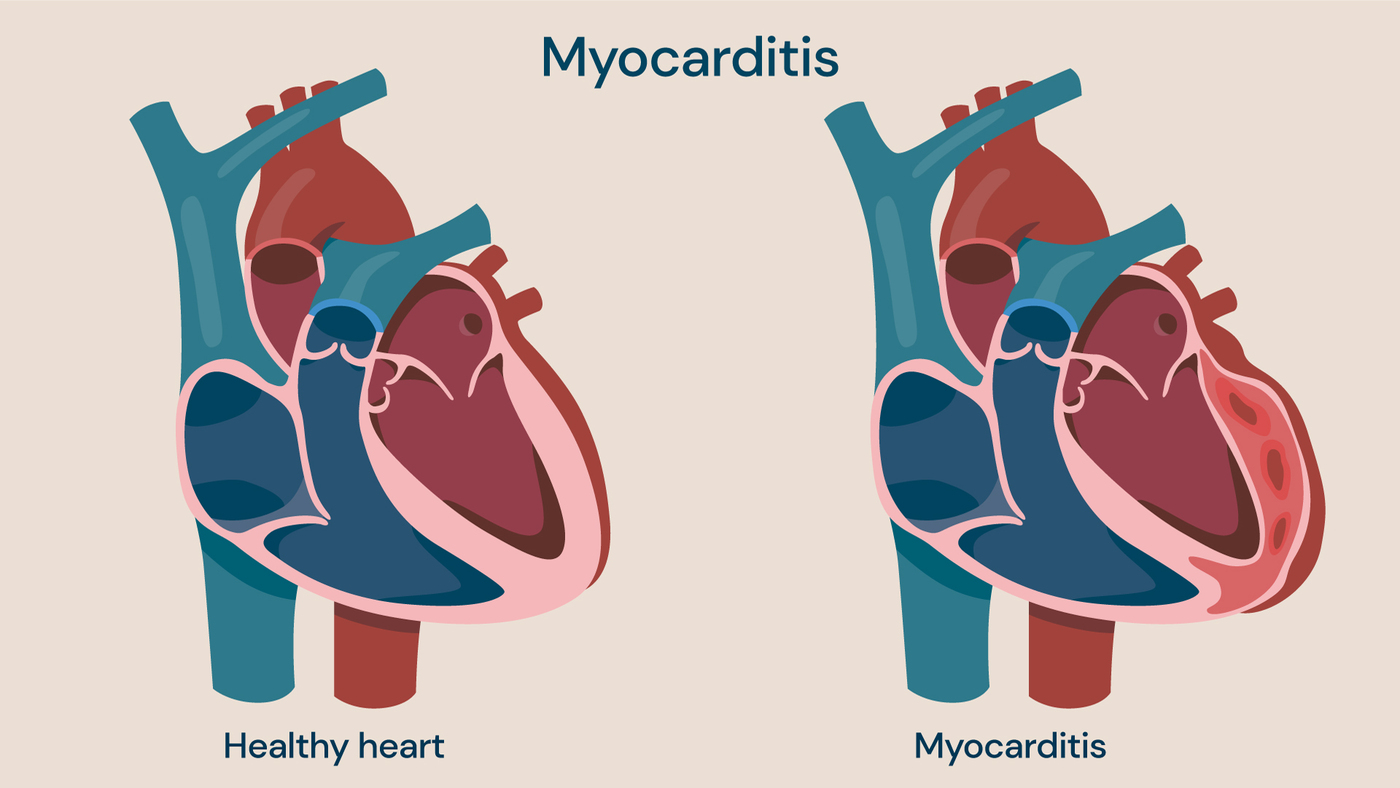
Myocarditis is inflammation of the heart muscle (myocardium), which reduces its ability to pump blood.
Types of myocarditis
There are several different types of myocarditis caused by a range of factors including infections, chemicals or even some drugs:
Acute myocarditis
This type of myocarditis can develop quickly, but symptoms usually resolve shortly after onset. It is typically caused by a viral infection and usually occurs in teenagers and infants, but it can occur at any age.
Chronic myocarditis
This type of myocarditis takes longer to treat, with symptoms frequently recurring. It tends to be caused by inflammatory conditions like autoimmune disorders when the immune system attacks cells and tissue.
Lymphocytic myocarditis
This is a rare type of myocarditis that occurs when lymphocytes (a type of white blood cell) enter the heart muscle and cause inflammation. Lymphocytic myocarditis can happen after a viral infection and may require hospitalisation.
Symptoms of myocarditis
Many people will feel no symptoms from myocarditis, and the condition will pass without them knowing that they had it. Other people will experience mild symptoms, which may include:
- tiredness, with physical activity becoming more difficult
- chest pain, a pressure, tightness or squeezing in the chest, either during activity or at rest
- irregular or rapid heartbeat (arrhythmias), due to the inflammation affecting the heart’s electrical system
- swelling of the legs and feet
- light-headedness, feeling dizzy or that you could faint
- shortness of breath
- flu-like symptoms, including fever, sore throat, body ache and headache
If you experience symptoms such as unexplained chest pain, shortness of breath, or a rapid heartbeat, you should seek immediate medical help. Occasionally the symptoms of myocarditis can mimic a heart attack.
Myocarditis causes
Myocarditis is uncommon and usually doesn’t require treatment as symptoms tend to subside after a short period of time.
However, there are several potential causes of myocarditis:
Viruses
A range of viruses can lead to myocarditis, including:
- common colds
- hepatitis B
- hepatitis C
- COVID-19
- parvovirus
- herpes
Viruses are the most common cause of myocarditis. The condition is caused by cells your body produces to fight the virus, which release chemicals that can inflame the heart.
Parasites
Parasites can be transmitted by insects, causing Chagas disease which can lead to thickening and scarring of the heart tissue. People from Central and South America are particularly at risk as this organism is common there.
Bacteria
Bacteria including streptococcus, staphylococcus and bacteria that causes Lyme disease can lead to myocarditis. This is an uncommon cause and is usually due to the body’s reaction to a bacterial infection (sepsis).
Fungi
If you have a weakened immune system, a fungal infection – including yeast infections, moulds and fungi contained in bird droppings – can cause myocarditis.
Myocarditis can also be caused by:
- medications including cancer drugs, antibiotics and anti-seizure medications
- illegal drugs
- exposure to radiation or chemicals
Long term effects of myocarditis
Myocarditis can usually resolve without permanent complications. However, in some cases, it can lead to serious complications. The potential complications of myocarditis include:
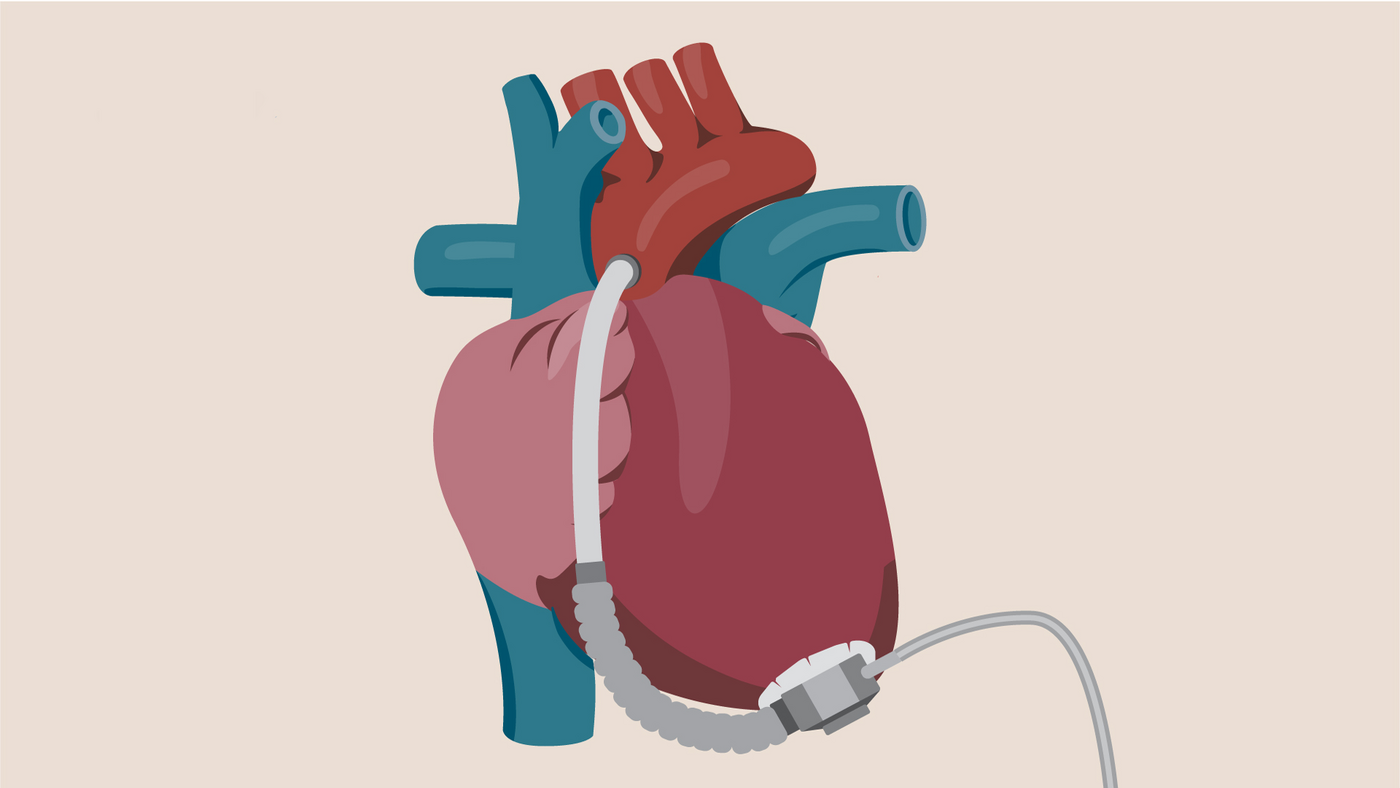
- Heart failure: if the condition persists, and is left untreated myocarditis can cause heart damage, with the heart muscle not able to pump blood properly. In some cases, a ventricular assist device may need to be worn, or a heart transplant may be required.
- Heart attack: when the heart muscle is injured, blood clots may form, leading to a heart attack or stroke.
- Irregular heart rhythm (arrhythmias): when the heart damage alters the way the heart beats.
- Cardiac death: which can be caused by serious irregular heart rhythms that stop the heart from beating. This is known as sudden cardiac arrest
Myocarditis diagnosis
When diagnosing myocarditis, your doctor is likely to carry out a physical examination and ask you questions about your medical history. There are also several tests which may be carried out to diagnose myocarditis, including:
- electrocardiogram: a cardiac test used to check your heart’s rhythm and electrical activity
- chest X-ray: shows shape and size of the heart and may demonstrate enlargement of the heart caused by the presence of fluid related to heart failure
- echocardiogram: a type of ultrasound scan typically performed to observe the heart and surrounding blood vessels
- magnetic resonance imaging (MRI): an advanced imaging test offering more detailed analysis and assessment of myocardial oedema (inflammation in the heart muscle)
- positron emission tomography (PET) scan: to provide metabolic (related to your body’s biochemical process) information on inflammation.
- cardiac catheterisation: an invasive cardiac test that analyses the function and structure of the heart, and allows the coronary arteries to be seen to exclude coronary artery disease
- endomyocardial biopsy: used to diagnose myocarditis in more than 30% of unexplained cases, this procedure obtains a small sample of myocardial (heart muscle) tissue for analysis
- blood tests: these tests are used to check for signs of infection, inflammation or a heart attack. It may be possible to detect antibodies to an infection linked to myocarditis, or to detect enzymes released by damaged heart muscle
Myocarditis treatment
Often, myocarditis does not require treatment since most cases resolve on their own. However, if you suffer from severe or chronic myocarditis, or experience symptoms such as shortness of breath or arrhythmias, medical intervention may be required.
There are a range of treatments available to treat myocarditis, depending on the type, severity and prognosis, from medication to surgery.
Medication for myocarditis
Medications for myocarditis include:
- heart medications: to reduce the risk of blood clots, for cases in which myocarditis is irregular heart rhythms or heart failure
- corticosteroids: to suppress your immune system, used to treat eosinophilic myocarditis, giant cell myocarditis and other rare forms of the condition
- diuretics: to help reduce the accumulation of fluid
- beta-blockers: to lower the heart rate
- angiotensin-converting enzyme inhibitors: to slow progression of cardiovascular disease
- angiotensin II receptor blockers: to help to lower blood pressure and prevent heart damage
- other medications: for chronic conditions that can cause myocarditis such as viruses and lupus (autoimmune disease)
the majority of patients will only require medication for a short time, some may develop permanent heart damage that requires life-long medication.
Surgery for myocarditis
There are several surgical options for severe myocarditis, which may be required to treat the cause and symptoms of the condition. These include:
- intra-aortic balloon pump: a device that inflates and deflates in the main artery to improve blood flow
- ventricular assist device (VAD): a device which can replace the function of a weak heart
- extracorporeal membrane oxygenation: using a machine that removes carbon dioxide and delivers oxygen to the blood
- a heart transplant: for severe myocarditis
Surgery for myocarditis
There are several surgical options for severe myocarditis, which may be required to treat the cause and symptoms of the condition. These include:
- intra-aortic balloon pump: a device that inflates and deflates in the main artery to improve blood flow
- ventricular assist device (VAD): a device which can replace the function of a weak heart
- extracorporeal membrane oxygenation: using a machine that removes carbon dioxide and delivers oxygen to the blood
- a heart transplant: for severe myocarditis
Locations
Discover our team of cardiac surgery experts
Meet our team of leading cardiac surgery specialists. From heart health to advanced interventions, our specialists are here to provide personalised care to you.