What is TEVAR?
TEVAR stands for Thoracic EndoVascular Aortic Repair. TEVAR is the recommended minimally invasive treatment for a weakened and/or dissected aorta. The aorta originates from your heart and it’s the main artery of the body, supplying blood to your circulatory system and all vital organs.
A weakened aorta might be caused by an aortic ulcer, a thoracic aortic aneurysm or an aortic dissection.
How does TEVAR work?
TEVAR is a procedure which is used to repair the aorta and provide inner support to its weakened sections. It relies on inserting a stent into the aorta to essentially scaffold the artery and remove pressure from its damaged parts.
This helps to prevent the aneurysm or ulcer from rupturing and also stops blood leaking between the layers of the walls of your arteries in the case of aortic dissection.
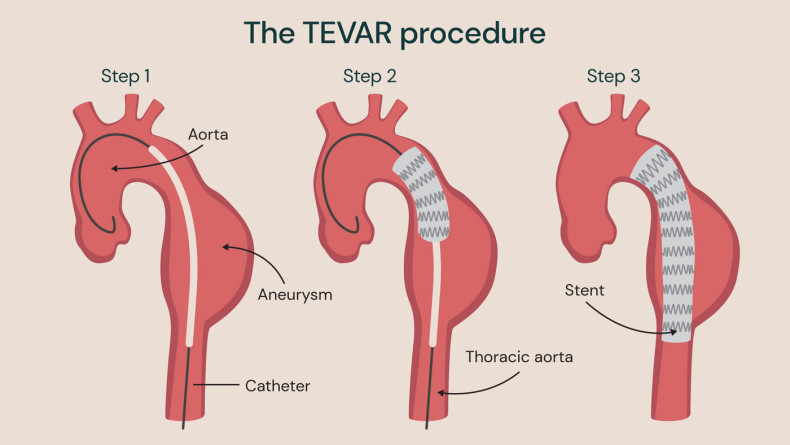
Standard TEVAR procedure for aortic aneurysm using one stent to support the aorta
What is an aortic ulcer?
An aortic ulcer is an irregularity of the aortic wall caused the build-up of plaque in the aorta. The plaque causes the inner lining of the aorta to wear down, gradually eroding the artery wall. If left untreated, it can increase your risk of developing an aortic aneurysm or aortic dissection.
Two of the main symptoms of aortic ulcers are chest pain and back pain which are often associated with a number of other heart problems. Unfortunately, this can make aortic ulcers difficult to identify, and a diagnosis might involve a CT scan or other imaging tests.
Symptoms of an aortic ulcer may include:
- chest and back pain
- high blood pressure
- weakness
Once identified, a CT scan can also be used to monitor the increasing size of an aortic ulcer.
What is a thoracic aortic aneurysm?
Aortic aneurysms can either be thoracic (relating to the chest) or abdominal. Depending on location and anatomical details, TEVAR treatment may be recommended for thoracic aortic aneurysms.
Within thoracic aortic aneurysms, there are two further sub-types; ascending and descending aneurysms, depending on the location within the aorta. An ascending aortic aneurysm occurs in the section of the aorta which extends upwards from the heart; for this section of the aorta, open surgery is almost always needed. A descending aortic aneurysm occurs in the section of the aorta which is in the lower part of the chest beyond the arch, and is often amenable for a TEVAR procedure.
All thoracic aortic aneurysms form when a part of the aorta becomes weak, bulges out and progresses to a balloon-like enlargement. Over time, aneurysms grow larger and, if left untreated, this can lead to various complications.
Complications commonly associated with aortic aneurysms are rupture, aortic dissection, compression of adjacent structures, and blood clots. Rupture is the most serious complication of aortic aneurysms, leading to life-threatening internal bleeding.
If an aortic aneurysm is identified before it causes complications and becomes an emergency, it can be monitored with regular scans and be effectively treated before it ruptures or causes further issues.
Symptoms of a thoracic aortic aneurysm are:
- chest or back pain
- abdominal pain
- shortness of breath
- difficulty swallowing
- hoarseness
What is aortic dissection?
Aortic dissection is a serious and often urgent condition whereby the inner layer of the aorta has a tear. This causes the inner and middle layers of the aortic wall to separate, allowing blood to rush into the tear, and accumulate in a newly formed false lumen. The inner and middle layers of the aorta then separate (or dissect), which can lead to rupture of the aorta if not treated promptly.
There are two types of aortic dissection – type A and type B. Type A dissection usually occurs in the part of the aorta which is closest to the heart. Type A dissection is usually immediately life-threatening, requiring urgent open surgery to repair the aorta or, in some cases, replace the affected section of the aorta.
TEVAR intervention is suitable for patients with type B aortic dissection which occurs further down the aorta, further away from the heart. Depending on the position of the dissection and how it affects blood flow, surgery for type B dissection isn’t always needed urgently. This allows more time for the patient to be recommended TEVAR surgery with a custom-made stent if required.
Symptoms of aortic dissection can vary depending on which type you have, but can include:
- chest or back pain with a tearing or stabbing sensation
- shortness of breath
- fainting
- weak pulse or pulse differential
- temporary loss of vision
- compromised blood flow to legs
- stroke symptoms
What happens in a TEVAR procedure?
TEVAR is a minimally invasive procedure which is carried out through a small incision in the groin area. The cardiologist or vascular specialist places a wire in the true lumen of the dissected aorta and directs a stent graft to the weakened section by passing the stent up your artery until it reaches the target spot of the aorta. The interventional cardiologist or vascular specialist then positions the stent graft exactly where the ulcer, aneurysm or entry tear of the dissection is located, supporting the aortic wall and preventing rupture.
The entire procedure is performed under general anaesthetic in just 90 minutes. For a fit patient, recovery time tends to be around two to three days. However, as most patients with aortic disease are aged 70 and older, their recovery time is often closer to five days.
What is a unibody single-branch stent?
In cases of aortic ulcers, aneurysms or dissections which don’t occur near the aortic arch, a standard TEVAR stent can be sufficient to treat the pathology.
However, when the ulcer, aneurysm or dissection occurs or originates in the distal aortic arch or near the left subclavian artery, a single standard TEVAR stent is not sufficient. In order to protect and preserve the left subclavian and left vertebral artery (one of the four blood vessels which supplies your head, neck and arms), an additional stent graft or a vascular bypass operation with an inherent risk is needed.
Although this need can be met by inserting a separate side-branch stent graft, it isn’t without risk. In 10-15% of cases, the two stents move slightly, allowing a gap to form between them (endoleak). This means that blood can leak in between, and further surgery may be required to correct this endoleak and prevent further complications or rupture in the future.
With a unibody single-branch stent, the additional branch is sewn into the main stent forming a unibody, with the single-branch directed into the subclavian artery to protect it. This means that the stent graft is manufactured in one piece, with no risk of blood leaking between side-branch and the main body of the stent graft.
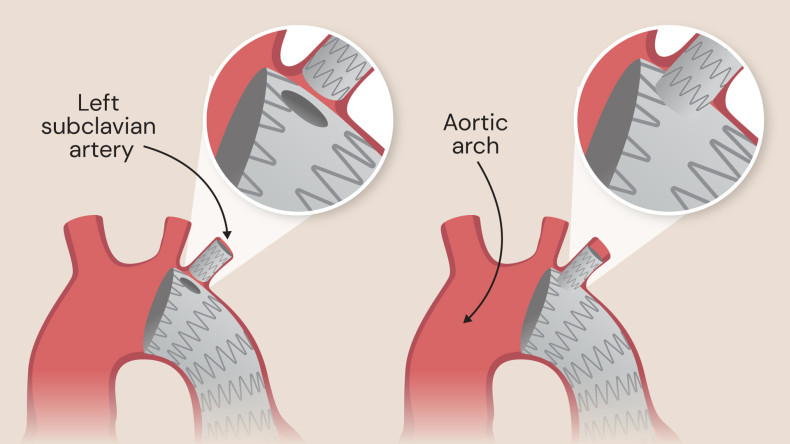
Standard separate side-branch (left) and unibody side-branch device (right)
Custom made stent grafts for personalised care
Before the TEVAR procedure can go ahead, you must have an ECG-gated CT scan to produce detailed images of your anatomy. These scans will give exact measurements for the size of your aorta and left subclavian artery, allowing the unibody stent to be manufactured or selected to perfectly fit your aortic arch.
The stent graft is made from nitinol surrounded by biocompatible fabric. It’s designed to redirect the blood steam to the true lumen in case of an aortic dissection, therefore protecting the aortic wall from any further damage. In cases of ulcers and aneurysms, the stent graft protects the diseased wall of the aorta from wall stress.
The actual stent is a scaffold-type structure made from nitinol. Nitinol is an alloy with temperature memory and the stent is designed to expand at 37 degrees (body temperature). This means that the stent can be passed up the artery while compacted, before expanding to its full extent once it’s in place in the aorta.
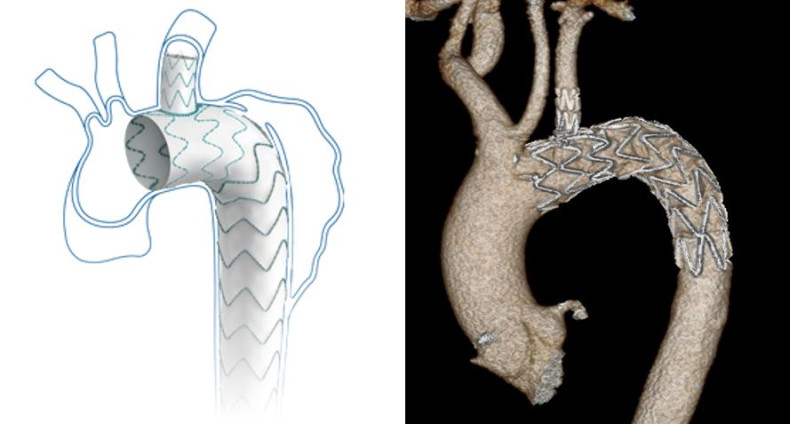
The manufacturer’s diagram of the unibody stent, and a scan depicting the stent in place in a patient’s aortic arch
The benefits of TEVAR and unibody single-branch stent graft
There are numerous benefits of having TEVAR with a unibody single-branch design. The procedure has been developed to protect and preserve the left subclavian artery with a quicker patient recovery in mind when compared with additional vascular bypass surgery. With this feature, the unibody stent is designed to avoid the risk of vascular bypass surgery to the neck or other interventions.
Advantages of having the TEVAR procedure without the vascular bypass surgery include:
- lower risk of complications, including infection
- reduced recovery time due to being minimally invasive
- preservation of left subclavian artery without neck surgery
- unibody single-branch design avoids endoleak
All things considered, using the unibody single-branch stent graft eliminates the risk of leakage between two individual stents. This reduces the chance of requiring further treatment to repair leaks in the future.
What are the risks of TEVAR?
No procedure is entirely risk-free, but TEVAR – especially using a unibody single-branch stent – is generally a safe procedure with a low risk profile. However, some complications of TEVAR can include:
- infection around the incision in the groin
- blood vessel injuries
- stroke due to a clot or dislodgement of debris
Contact us
To learn more about our strategy with TEVAR procedures in the setting of aortic dissection, aneurysm or aortic ulcer, please get in touch with our customer services team. They can provide further information and help you to book an appointment with our specialist consultants.
