Many of us experience trouble sleeping from time to time but if you feel continuously tired during the day even after a full night’s sleep, it may be a sign of a condition called sleep apnoea. Loud snoring is the most common symptom and the condition can be harmful to your heart, but our world-leading sleep specialists can diagnose and treat the condition quickly, to help you sleep peacefully again.
What is sleep apnoea?
Sleep apnoea (ap-nee-uh) is a relatively common condition where your breathing is interrupted during sleep. Your breathing can stop and start repeatedly, sometimes hundreds of times a night.
“The condition can be serious if left untreated and result in a range of health problems. These include high blood pressure, diabetes, and heart problems, such as an irregular heartbeat – called atrial fibrillation, heart attacks and stroke.” explains our consultant physician in respiratory and sleep medicine, Dr Allie Hare.
“If you have sleep apnoea, you may snore loudly and feel tired or have trouble concentrating during the day even after a full night’s sleep. Daytime sleepiness can increase the risk of road traffic accidents and accidents at work.”
Our world-leading sleep experts, such as Dr Hare, can diagnose and treat the condition quickly. If you think you might have the condition, get in touch with our team who can book you an appointment with one of our consultants.
What causes sleep apnoea?
Obstructive sleep apnoea is the most common form of the condition. This occurs due to narrowing and closure of the upper airway in the throat, during sleep. Anything which makes the upper airway narrower will increase the tendency for it to close during sleep – for example, enlarged tonsils, a set-back lower jaw, or increased weight or musculature in the neck area.
When the upper airway narrows or closes in sleep, the flow of air to the lungs is reduced, or stops completely, lowering the oxygen levels in the bloodstream. Your brain is very sensitive to the lower oxygen levels, and will wake you up, or rouse you into a lighter sleep stage, so that the neck muscles wake up and open the airway. The flow of air then restarts (often with a loud gasp or body jerk), the oxygen levels increase and you can return to sleep, when the whole process can start again. This can happen 30-50 times an hour or more, in severe cases.
This repeated drop in oxygen levels overnight can interfere with your sleep, reduce the amount of oxygen getting to your organs and cause problems with your blood pressure and your heart’s rhythm.
Central sleep apnoea is another, less common, form of the condition. This occurs when your brain fails to send signals to your breathing muscles causing you to stop breathing for a short period. Some people may have a mixture of both conditions, called ‘complex sleep apnoea syndrome’.
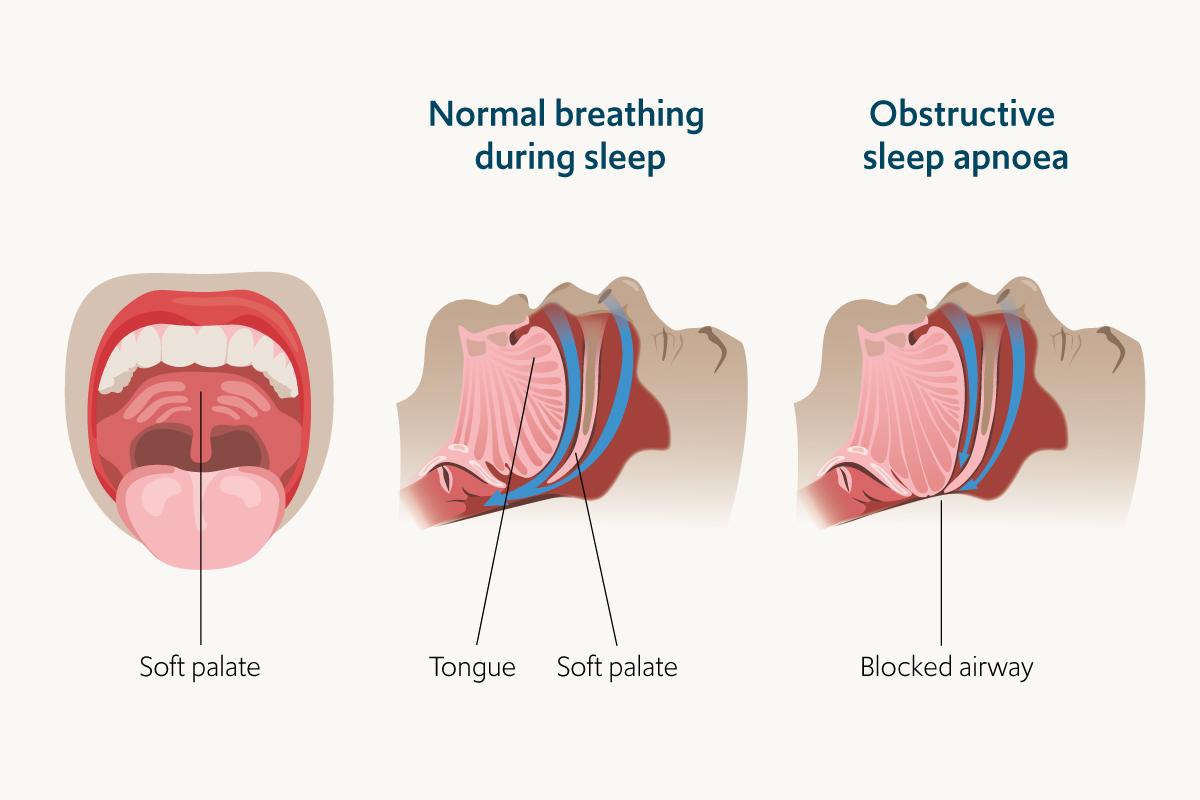
Obstructive sleep apnoea occurs when the upper airways of the throat temporarily close during sleep
What are the symptoms of sleep apnoea?
The symptoms of obstructive and central sleep apnoea overlap, making it challenging to diagnose which type you have. The most common symptoms of both types are listed below:
- loud snoring
- breathing stopping and starting repeatedly – which is often reported by someone else, such as a partner who sleeps beside you
- waking up frequently
- making snorting, gasping or choking noises in sleep
- difficulty staying asleep (insomnia)
- feeling very tired and sleepy during the day (hypersomnia)
- finding it hard to concentrate while awake. Patients with sleep apnoea are at an increased risk of workplace and car accidents
- feeling irritable or low in mood
You should speak to your doctor if you think you might have sleep apnoea.

The most common symptom of sleep apnoea is loud snoring, which is normally picked up by a partner sharing your bed
Who gets sleep apnoea?
There are different factors that increase the risk of obstructive sleep apnoea and central sleep apnoea.
For obstructive sleep apnoea, risk factors include:
- excess weight – obese people are at an increased risk
- gender – men are two to three times more likely to have the condition than women. However, menopause and gaining excess weight can increase the risk in women
- smoking – smokers are three times more likely to have the condition than people who have never smoked
- age – your risk of obstructive sleep apnoea increases with age
- a family history of obstructive sleep apnoea
- neck anatomy – you may have inherited a narrow throat, or larger tonsils or adenoids may block airways (particularly in children). People with larger necks may also have narrower airways
For central sleep apnoea, risk factors include:
- age – middle-aged and older people are at increased risk
- gender – the condition occurs more commonly in men than women
- heart disorders, such as congestive heart failure
- taking narcotic pain medications, such as opioid ‘morphine-type’ medications
- stroke – having had a stroke previously increases the risk of getting the condition

Men and individuals who are obese are at an increased risk of sleep apnoea.
How is sleep apnoea diagnosed?
If your doctor thinks you may have sleep apnoea, they will refer you to a sleep specialist like Dr Allie Hare for an evaluation. You can also book an appointment directly with one of our sleep specialists yourself, if you think you might be experiencing symptoms of sleep apnoea.
During your initial appointment with one of our consultants, they will evaluate your symptoms and sleep history – someone who shares your bed or household can help you with this. For example, they can confirm if you snore or experience any other symptoms that you may not be aware of while asleep.
Depending their initial evaluation, our sleep specialists may recommend a sleep study. A sleep study is an overnight assessment of your breathing and other body functions during sleep and helps our consultants with their diagnosis.

Royal Brompton Centre for Sleep in Chelsea, London
There are two types of overnight sleep study:
- Nocturnal polysomnography. This study is performed at our Royal Brompton Centre for Sleep in Chelsea. Our team will attach a range of sensors to your chest, finger and upper lip to measure your oxygen levels, breathing and movements of your chest and abdomen. Our specialist team will check on you while you sleep to make sure your sleep study is completed successfully
- Home sleep study. Depending on your health background, you can complete a sleep study in the comfort of your own home if you wish to. You will be provided with medical devices that measure your blood oxygen levels, airflow, breathing patterns and heart rate. We will then review your recordings and make an assessment when the medical devices are sent back to us
How is sleep apnoea treated?
Our sleep specialists may recommend a range of treatment options for your sleep apnoea, depending on the severity of your condition.
Lifestyle changes
For mild sleep apnoea, you may be recommended to undertake some lifestyle changes, such as quitting smoking and losing weight. If you have allergies which affect your breathing, our specialists may recommend treatment for your allergies.
If your sleep apnoea doesn’t improve with lifestyle changes, or your sleep apnoea is moderate to severe and you have daytime symptoms and/or sleep disturbance, our consultants may recommend other treatments such as devices that can help keep your airways open while sleeping.
Continuous positive airway pressure (CPAP)
The most common and reliable method for treating moderate to severe sleep apnoea is called a continuous positive airway pressure (CPAP – pronounced ‘SEE-pap’) machine. The CPAP machine works to deliver air at pressure through a mask that is placed over your nose and/or mouth. This helps keep your airways open while you sleep to prevent sleep apnoea and snoring.

A patient using a continuous positive airway pressure machine
Oral devices
Some patients may find CPAP machines uncomfortable at first, but with practice, most learn to adjust to using them while sleeping. However, if you continue to struggle to use a CPAP machine, or your sleep apnoea is less severe, oral devices are another option that our sleep specialists may recommend.
Oral devices (also called mandibular advancement devices) are designed to keep your throat open when worn while sleeping and may be a suitable option for mild to moderate sleep apnoea. They work by preventing the tongue from blocking the throat and/or move the lower jaw forward to keep your throat open. Although oral devices may be easier to use, CPAP is more reliably effective for more severe sleep apnoea.
Surgery
If other sleep apnoea treatment options have failed, our sleep specialists may recommend review by a specialist Ear, Nose and Throat (ENT) surgeon. This is normally only considered after trialling other treatments for at least three months but can be recommended as the first treatment option for people that have particular issues with the structure of their jaw or upper airway.
A surgeon may recommend the removal of your tonsils or adenoids, or other tissues from the back of your mouth or top of your throat if they feel this could prevent the blocking of your airways while sleeping. Our consultant team have close relationships with a number of specialist surgical colleagues who are experts in sleep apnoea surgery.
Get in touch
If you think you may have sleep apnoea and would like to speak to one of our sleep specialists like Dr Allie Hare, get in touch with our team to see how we can help you.
Related content
-
Sleep disorders
There are many types of sleep disorders - both common and complex - including sleep apnoea, narcolepsy and parasominas. Learn more.
-
Sleep disorder clinic
Our experts treat all sleep disorders and can create tailored programmes of care to reduce symptoms and significantly improve quality of life.
-
Sleep medicine
We have been diagnosing and treating adult sleep conditions for over 20 years at Royal Brompton and Harefield hospitals - the largest sleep service in Europe.
