A high-risk pulmonary embolism can be fatal if not treated promptly. Our radiology specialists use advanced dual-energy CT to rapidly diagnose the presence, location and extent of the clot most accurately in the lungs and offer two minimally invasive procedures to treat the condition.
The EkoSonic Endovascular System used to treat a high-risk pulmonary embolism.
Pulmonary embolism: A life-threatening problem
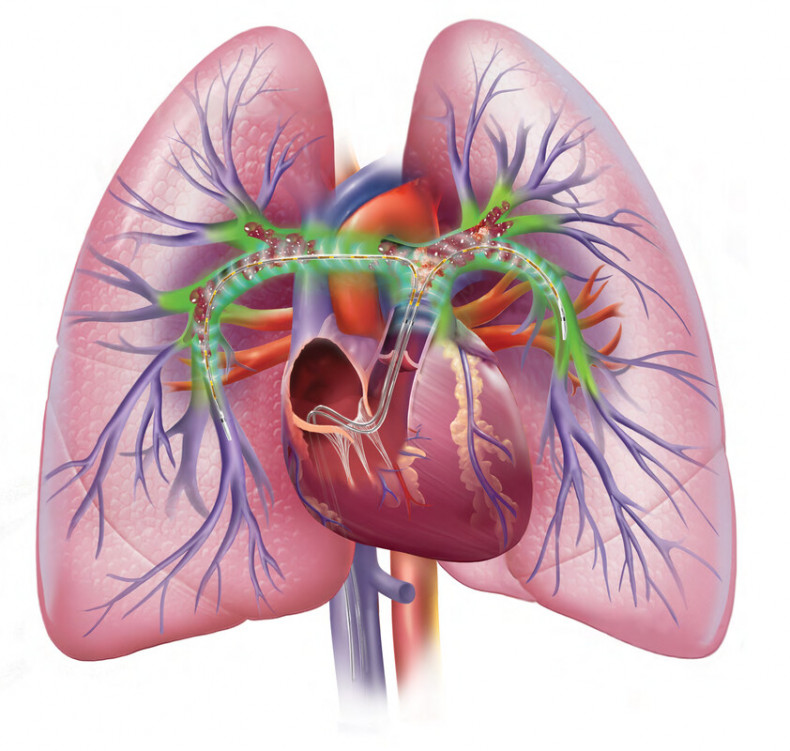
A pulmonary embolism (PE) can occur when one or more emboli – usually arising from a blood clot in the deep veins of the legs – become lodged in the pulmonary arterial system.
The exact prevalence of the condition is unknown as PE can be challenging to diagnose with a wide spectrum of symptoms- ranging from asymptomatic, in the case of small PE, to sudden death if the PE is large.
Across this spectrum, PE is one of the most common cardiovascular diseases in developed countries – third only to heart attacks and strokes.
In the UK, the annual incidence of diagnosed PE is 7-8 per 10,000 people, with 47,594 cases reported during the 1-year period between 2013 and 2014 (the most recent report).
High-risk PE occurs when the pulmonary circulation is suddenly obstructed. To compensate for this, the right ventricle works harder to increase pulmonary systolic pressure. This puts strain on the thin-walled right ventricle which normally works against low pressure.
If this increase in right ventricular output cannot be sustained, it can lead to right heart failure and death. The overall mortality rate for high-risk pulmonary embolism can reach up to 65%, with treatment lowering this to 20%. It is therefore imperative that patients receive treatment to remove the obstruction swiftly.
The clinical classification of PE severity is based on mortality risk. This classification determines the type of treatment patients receive. “High-risk” PE is defined as a PE which causes a sustained systolic blood pressure less than 90 mmHg. In this situation, reperfusion is the goal of care, either through systemic (i.e. thrombolytic) or localised treatment of the PE (i.e. surgical or catheter-directed therapies).
If patients do not exhibit systolic hypotension but exhibit other features of shock and/or have pre-existing conditions which may contribute to a worse outcome, this is assessed using a PE severity index (PESI) and if this score is significantly elevated, the patient may be stratified as “Intermediate-high-risk”.
Intermediate-high-risk PE consists of relative hemodynamic stability with a high PESI score, right ventricular dysfunction, and positive cardiac biomarkers. Intermediate-high-risk PE is primarily treated with anticoagulation. If, however, anticoagulation is contraindicated, or if haemodynamic compromise develops, catheter directed therapies are recommended.
Improving diagnostic accuracy with dual-energy CT
Given the broad range of symptoms experienced with acute PE, clinical evaluation can be limited in achieving a diagnosis.
Some clinical features can increase the likelihood of PE, including a family history, certain cancers (such as lung and ovarian cancer), long-term immobility (such as that experienced with long-haul flights and prolonged bed rest), pregnancy, oral contraceptive therapy and COVID-19 infection.
“When a pulmonary embolism is suspected, it is important that patients are assessed by a doctor as soon as possible to confirm the diagnosis and determine the severity of PE” explains our cardiothoracic and interventional radiologist, Dr Carole Ridge.
“At Royal Brompton and Harefield hospitals, we have expertise in dual-energy CT pulmonary angiography – a specialist diagnostic tool which accurately diagnoses the presence, location and extent of a pulmonary embolism. This technique helps develop the best treatment strategy and has been particularly useful in the case of high-risk PE.”
Dual-energy CT is an advanced imaging technique which helps detect PE. Unlike standard CT scanners which use polyenergetic X-rays to form a cross-sectional image of a patient’s anatomy, a dual-energy CT scanner uses two X-ray beams of varying peak energies to form a map of lung perfusion.
This combination of X-rays enables the scanner to localise the contrast agent, iodine, in the lungs and create detailed images of the small blood vessels in the lung so that physicians can assess the effect of a PE. In fact, when comparing dual-energy CT with conventional CT angiography in the diagnosis of PE, one recent publication in over a thousand patients demonstrated that a review of these dual-energy perfusion maps helped detect 2% more PEs than found using conventional CT images alone.
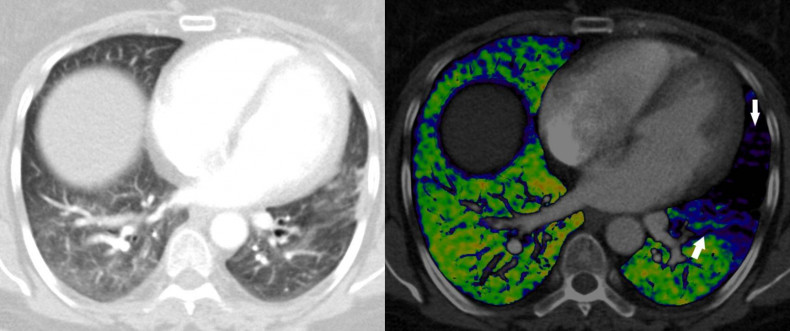
Increased PE clarity with dual-energy CT. (Left) A conventional CT angiography scan of a patient with a pulmonary embolism in the left lung. (Right) A dual-energy CT scan of the same patient with arrows indicating the location of the pulmonary embolism visualised more clearly in black. The right lung is well supplied by blood vessels shown in green.
Two specialist minimally invasive approaches to treatment
We offer two minimally invasive procedures at Royal Brompton Hospital for patients with high-risk or intermediate-high-risk PE. They can be used as standalone treatments or in combination depending on the condition of the patient.
Catheter-directed acoustic pulse thrombolysis
Systemic thrombolysis has been consistently shown in randomised controlled trials to rapidly improve right ventricular function in patients with high-risk PE. However, it also significantly increases the risk of bleeding complications. In treatment registries, systemic thrombolysis has been associated with major bleeding rates as high as 20% and intracranial haemorrhage in up to 3%.
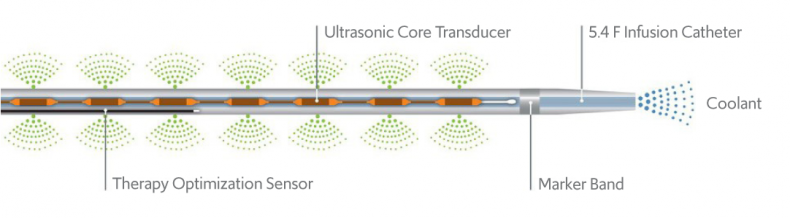
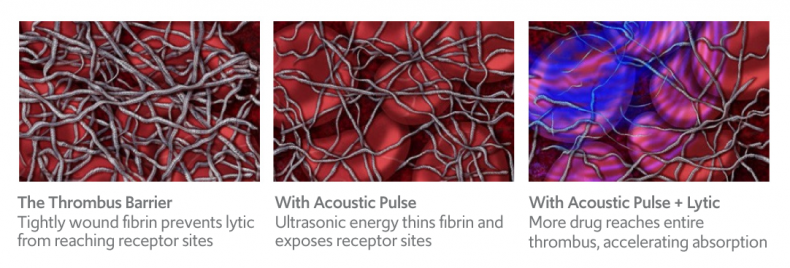
The EkoSonic Endovascular System enables thrombolytic drugs to be delivered locally to the pulmonary embolism and an acoustic pulse helps accelerate absorption of the drug and its thrombolytic effect.
The EkoSonic Endovascular System offers an alternative approach to systemic thrombolysis. It is a catheter-based system that can deliver thrombolytic agents directly to where they are needed with ultrasonic core elements that delivery ultrasound energy locally.
The EkoSonic Endovascular System’s ultrasound waves accelerate clot dissolution.
The acoustic pulse generated by the ultrasonic core causes fibrin within the clot to fragment. This enables thrombolytic agents to enter more deeply into the clot and exposes plasminogen receptor sites to accelerate the absorption and thrombolytic effect of the agent when compared to catheter-based delivery alone.
Trials have demonstrated a rapid reduction in right ventricle strain and pulmonary arterial pressure with this system. The right ventricular-to-left ventricular (RV/LV) ratio is reduced by 23% on average within 2 hours and pulmonary arterial pressures by 28% within 48 hours.
The acoustic pulse also enables the thrombolytic drug dose to be reduced by 76% when compared to standard treatment. A low risk of bleeding has also been reported.
“For patients that are not suitable for thrombolysis, such as those at increased risk of bleeding, mechanical aspiration thrombectomy is an alternative option to treat high-risk PE,” explains Dr Ridge.

The Penumbra Indigo thromboaspiration system.
The Indigo thromboaspiration system offers an advanced approach to treating pulmonary embolism by achieving thrombectomy with or without the use of thrombolytic drugs. Powered by a vacuum pump, the system works in conjunction with an 8 Fr catheter to deliver powerful aspiration and actively remove thrombus.
In the 2019 EXTRACT-PE study, a recent prospective, single-arm, multicentre study on patients with high-risk PE, the Indigo aspiration system was shown to reduce right ventricular dilatation within 48 hours and avoid the need for thrombolysis in 98.3% of patients. There was also a low incidence of life-threatening complications associated with this device.
“We are pleased to be able to offer these two different minimally invasive procedures to treat high-risk pulmonary embolism at our hospital, enabling us to tailor treatment to the needs of our sickest patients” says Dr Ridge.
“For the best results, patients are assessed by our team of experts in radiology, intensive care and pulmonary hypertension medicine.”
Helping a COVID patient get back home

As a journalist, Bill was used to covering stories about others, but it was his own experiences of COVID-19 infection that made him the subject of national news last year.
Following some breathing complications associated with the infection, he was admitted to West Middlesex University Hospital for treatment and monitoring. “Although I’m in my 50s, I was relatively fit and healthy and thought I would get better with a bit of oxygen and rest,” Bill explains.
Unfortunately, his condition rapidly deteriorated and the medical team advised him that he would need to be sedated and transferred to Royal Brompton Hospital to be placed on ECMO life support.
While on ECMO, Bill experienced a range of complications due to the infection, including a high-risk pulmonary embolism.
“Bill was already in a very critical condition when he suffered from high-risk pulmonary embolism. Luckily, he was under the watchful eyes of our ECMO consultant, Dr Brijesh Patel, who spotted the change quickly,” explains Dr Ridge.
“We used the acoustic pulse thrombolysis catheter to break down the pulmonary embolism and are pleased to report the treatment was a success.”
Bill was on ECMO life support for a total of 32 days at our hospital. Months after leaving our hospital, he is still suffering from the long-term effects of his illness including problems with his heart, lungs and walking. However, he remains positive.

Bill having a lung function test at Royal Brompton Hospital as part of monitoring his recovery.
“I was unconscious throughout most of my stay at Royal Brompton Hospital, but I know that I am still here because of the life-saving treatment I received from their team who dutifully watched over me night and day,” says Bill.
“I still have a long road ahead of me in my recovery, but I am so grateful to still be under the care of the team at Royal Brompton.”
Contact us
For more information or to book an appointment, please contact our customer care team.

