It can be worrying to find out that you have mitral valve problems – but effective treatments are available. Medication can ease distressing symptoms, and specialist surgery can repair or replace your faulty mitral valve. In this article we explore the symptoms and treatments in more detail.
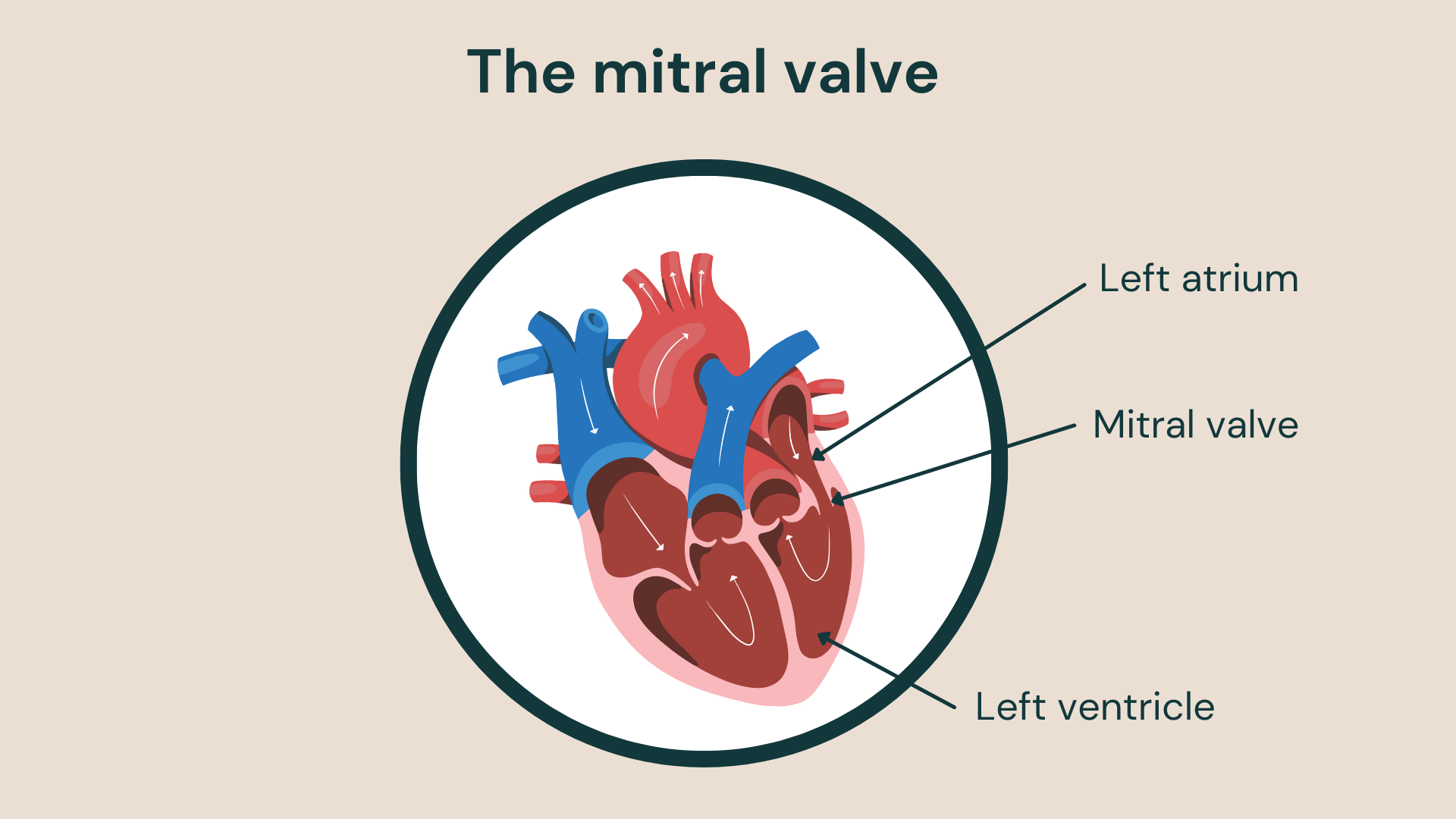
What is the mitral valve?
“The mitral valve is a complex structure that acts as a gateway between the left atrium and left ventricle, which are chambers of the heart. It lets blood flow between the chambers and prevents flow backwards,” explains our consultant interventional cardiologist, Dr Robert Smith.
The valve comprises two small flaps of tissue that open and close as your heart beats. When your left ventricle relaxes, the valve opens to allow blood to flow into the left ventricle from the atrium. The valve should close tightly when the ventricle contracts to stop blood from leaking back into the atrium.
What are mitral valve problems?
The mitral valve is one of the heart valves most vulnerable to problems. Valve problems develop when the valve can’t function properly because of disease, damage or age-related deterioration.
Mitral valve problems affect the normal flow of blood through the heart. Your heart has to work harder to pump blood around your body and supply the blood and oxygen to your organs and tissues. Over time this can progressively damage your heart and cause dangerous complications.
There main mitral valve problems are:
- mitral valve prolapse and regurgitation
- mitral stenosis.
Mitral valve prolapse and regurgitation
“Mitral regurgitation is a valve problem where the mitral valve does not close tightly. When the left ventricle contracts to pump blood around the body, blood leaks backwards into the left atrium,” explains Dr Smith.
Common causes of mitral regurgitation include:
- mitral prolapse or ‘flail’ due to degeneration of the valve support (chordal rupture)
- damage during or after a heart attack (ischaemic mitral regurgitation)
- leakage due to dysfunction and enlargement of the left ventricle (secondary mitral regurgitation)
- enlargement of the supporting mitral valve annulus (ring) due to atrial fibrillation
- damage by rheumatic fever following a streptococcal throat infection
- endocarditis (infection or inflammation of the valve).
Younger people can inherit a propensity to mitral valve prolapse that can develop into regurgitation at an earlier stage. Rarely children can develop mitral regurgitation due to congenital heart abnormalities.
Mitral regurgitation typically comes on gradually – but you may suddenly develop a valve problem if the supporting chord attaching the valve to the heart wall snaps. This can also occur suddenly after a heart attack. This medical emergency requires surgery to replace or repair your damaged valve.
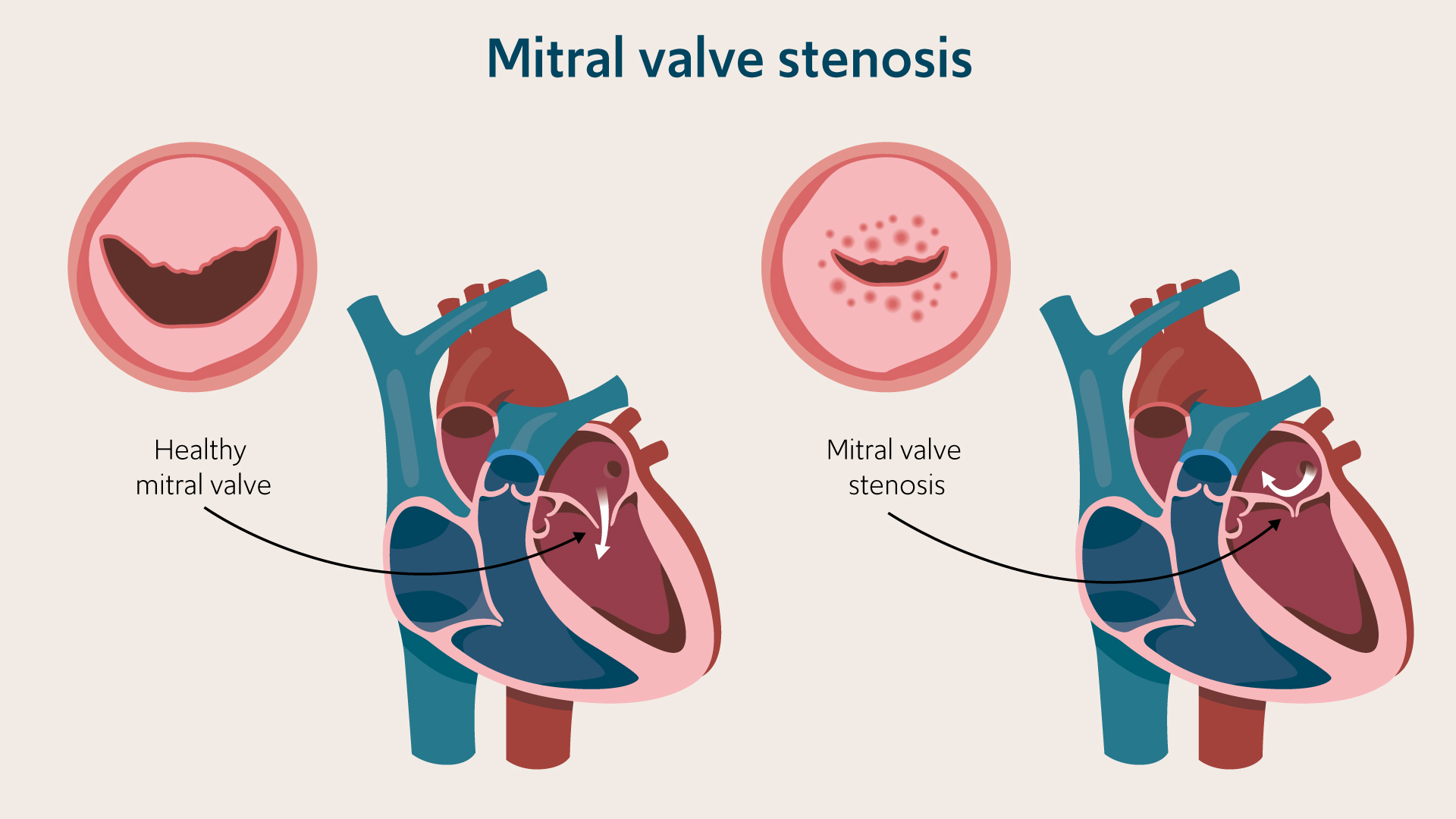
Mitral stenosis
“In mitral stenosis, your mitral valve becomes stiff and narrow, which restricts blood flow through the valve. Blood can back up in the atrium and lungs, which can cause heart rhythm abnormalities and fluid accumulation in the lungs,” explains Dr Smith.
Mitral stenosis is the most common type of valve problem across the globe. It is a particular problem in developing countries, where it develops due to rheumatic fever infection. Rheumatic fever can occur after streptococcal throat infection; it can scar the mitral valve, narrowing it and making it vulnerable to calcium deposits that increase stiffness. The valve may also leak. The widespread use of antibiotics has significantly reduced the incidence of mitral stenosis in industrialised countries.
Symptoms of mitral valve problems
Many people with mitral valve problems have no symptoms; your valve disease may be picked up on random screening, health checks or during treatment for another condition. However, if you have mitral valve problems, you may notice symptoms including:
- shortness of breath
- weakness and fatigue
- feeling dizzy, faint or lightheaded
- palpitations or irregular heartbeat
- swelling or your ankles, legs or abdomen
- chest pain
If you develop complications such as congestive cardiac failure, you may notice:
- breathlessness on exertion and when lying flat
- coughing
- coughing up blood – particularly with mitral stenosis
If the valve disease is untreated, it can lead to progressive heart failure and abnormal heart rhythms (e.g. atrial fibrillation). These conditions can lead to death. However, many people with mitral valve problems have no or little in the way of symptoms, especially in the early stages.
Diagnosis of mitral valve problems
If you are worried about your heart health, make an appointment with your GP or a specialist cardiologist. Experienced physicians can recognise valve disease by listening to your heart with a stethoscope. If you have mitral valve problems, they may hear abnormal sounds, including clicks and murmurs characteristic of a specific mitral valve problem.
If your specialist suspects a valve problem, they may recommend diagnostic tests such as:
- echocardiography: en ‘echo’ test is an ultrasound of the heart. A probe sends sound waves that bounce off your heart’s structures. It produces moving images of the heart and can show problems with the mitral valve, including whether it’s opening correctly, if there is blood flowing backwards, or if the valve bulges back into the atrium when it closes
- ECG: an electrocardiogram records and prints a trace of your heart’s rate, rhythm and electrical activity. It can show heart rhythm abnormalities, such as atrial fibrillation, which are more common if you have valve problems
- transoesophageal echocardiogram (TOE): A specialist echo that scans the heart from inside your oesophagus. The probe can get closer to the mitral valve so that the scanner gets more detailed information about the structure and function of the valve
- chest X-ray: May show heart enlargement and fluid in the lungs
- cardiac MRI: a cardiac MRI, or CMR, is a non-invasive diagnostic test used to scan the heart’s chambers, valves, blood flow and muscles to determine how well they function. It is particularly useful at assessing the myocardium (heart muscle)
- stress tests: an exercise ECG or stress echo can show how your heart works when it is ‘stressed’ by either exercise or specific medication
angiography: you may need an angiogram which looks at the heart’s blood supply and flow if the other investigations don’t provide sufficient information - right heart catheter: this is often undertaken at the same time as the angiogram. It involves a tube being advanced through a vein in the arm or groin. Its purpose is to measure the pressure within the heart and lung to further assess the severity of the valve disease and advise on the risk for surgery or other intervention
Treatment of mitral valve problems
If you don’t have any symptoms from your mitral valve problem, you may not need treatment. The right treatment will depend on your valve problem and your general health but can include:
- lifestyle changes to improve your heart health such as stopping smoking, reducing caffeine, and cutting back on alcohol
- medication to treat symptoms, such as:
- beta-blockers to help slow down an irregular heartbeat
- diuretics to get rid of excess fluid and treat breathlessness
- anti-hypertensive drugs to lower blood pressure
- blood thinners to prevent clots
- mitral valve repair surgery: open heart surgery to repair the valve and help it work more effectively
- minimally invasive repair surgery: this involves a small incision in the chest and can be truly ‘keyhole’ if it is carried out endoscopically and guided by a camera inside the chest
- mitral valve replacement surgery: open heart surgery to replace the mitral valve with a prosthetic device. This can also be achieved by a
- minimally invasive approach, where appropriate
- percutaneous mitral valve repair: minimally invasive procedure for example transcatheter edge-to-edge repair (TEER) to attach a clip to the mitral valve to help it close properly (e.g., with MitraClip or Pascal devices)
- balloon valvuloplasty: a minimally invasive procedure to open up the mitral valve and relieve the blockage
- transcatheter valve replacement – this is a developing technique that involves replacing the mitral valve through a small incision in the chest or groin. Currently, this technique is only an option for a small number of patients, but this may change as the devices and techniques develop
Get in touch
For more information or to book an appointment, please contact our customer care team.
