Management of lung cancer can be complex when most commonly diagnosed in the advanced stages. Our team of specialists can help screen and detect lung cancer in its earliest stages for a better chance of treatment success and offer various minimally invasive procedures to remove and control the spread of the disease.
Lung cancer: The global burden
Most deaths caused by cancer worldwide are due to that of the lung. It is responsible for almost 1 in 4 (1.6 million) cancer-related deaths each year – this is more than colon, prostate and breast cancer combined.
It is well known that most cases of lung cancer are due to smoking, but there is evidence that small dust-like particles in air pollution are also linked. It is not fully understood how these particles can damage DNA in cells to cause cancer, but the smallest particles known as PM10 and PM2.5 are known to be associated.
Workplace exposures may also contribute to an increased risk. These include exposure to asbestos during building work; silica during glass making or bricklaying; and regular exposure to diesel exhaust fumes – such as that experienced by professional drivers and mechanics.
Lung cancer increases with age and disease rates increasing sharply after 45. Symptoms of lung cancer are often non-specific and can include a persistent cough and/or breathlessness, coughing up blood, unexplained weight loss or tiredness and aches or pains when breathing or coughing.
Doctors may recommend a chest X-ray as the first test for lung cancer if patients are experiencing any of these symptoms and are thought to be at risk. If a nodule or ‘spot on the lung’ is seen in the X-ray, it can be a sign of lung cancer but may also be something else less serious. Further analysis by a specialist, including a CT scan to create more detailed images, will be needed to understand if it is lung cancer.
However, symptoms of lung cancer unfortunately often appear late, meaning that patients are usually only diagnosed at an advanced stage. For this reason, lung cancer survival rates remain low despite great advancements in treatment options.
Further, treatment can be complicated by other lung diseases that commonly appear alongside lung cancer, such as emphysema and/or chronic obstructive pulmonary disease (COPD). These conditions make breathing more difficult and are also linked to smoking and air pollution, as well as workplace exposure to chemical fumes and dust (e.g. from mining, or processing cotton, grain or wood).
Due to the complexity of the disease and it often presenting at an advanced stage, a specialist team is key to developing the most effective treatment strategy for each patient.

Air pollution, such as that caused by exhaust fumes from diesel cars, can increase the risk of lung cancer.
A team of experts behind every patient
As one of the world’s leading heart and lung care centres, we diagnose and treat hundreds of lung cancer patients each year, with many coming from other countries just to see our experts privately.
Each patient case is reviewed by multiple specialists rather than just one, as part of a ‘multi-disciplinary team meeting’. These meetings were first mandated by the UK National Cancer Plan in 2000 as a new gold standard of care for cancer patients in the NHS but are now an integral part of care delivery for all patients at our hospitals, regardless of their condition and are held twice weekly.
“Rather than patients having to seek a second opinion for their treatment, this is automatically built into our care pathways. They not only get a second opinion, but often a third, fourth and fifth expert all in the same room – from diagnostic to surgical specialists – offering their opinions on the best treatment strategy for a patient,” explains our consultant thoracic surgeon, Professor Eric Lim.
“For example, our world-renowned lung imaging and histopathology specialists can diagnose the type, location and stage of cancer with the greatest accuracy to help guide our thoracic surgeons on the best approach to surgical removal of the cancer with minimal harm to healthy lung tissues. This coordinated approach to care greatly improves the outcomes for each patient.”
Our centre has been identified as having one of the highest survival outcomes in lung cancer surgery by Getting It Right First Time. This is a national programme in the UK which aims to improve medical care within the NHS by identifying changes to services that can improve patient outcomes and sharing best practice between trusts.
We also collaborate with cancer specialists at the renowned Royal Marsden Hospital, where they provide expertise in chemotherapy, radiotherapy and immunotherapy treatment for our patients. Our specialists, in return, provide expertise in thoracic surgery procedures, including minimally invasive procedures, for all their lung cancer patients.
In addition, as our patients rarely present with one medical condition in isolation, our consultant respiratory physicians and cardiologists also offer expertise in treating other heart and lung conditions patients may have, such as emphysema, COPD and coronary artery disease, for a holistic approach to care.
One area of increasing importance is the field of cardio-oncology (heart health in cancer patients). Medical advances have led to patients surviving cancer-free for many years after treatment but life-saving treatments such as chemotherapy, can result in harm to the heart and blood circulatory system – called ‘cardio-toxicity’. Our experts can identify patients at highest risk of cardiotoxicity before they start treatment, so that we can take measures to best protect their hearts and blood circulatory system.

Our multi-disciplinary teams work together to share expertise and ensure the best outcomes for our patients.
Enhanced lung cancer screening
The chances of survival with advanced lung cancer are unfortunately low at just 20%. It is therefore important to capture the disease in its earliest stages for the greatest chance of treatment success.
Our lung cancer risk assessment service offers those at an increased risk of developing lung cancer (such as those aged over 50 and a long history of smoking) or worried about the symptoms (such as a persistent cough or dull ache in the chest) the chance to be comprehensively reviewed by one of our specialists in respiratory medicine.
Following the assessment, patients may be recommended to have a low dose chest CT scan. This imaging test can detect lung cancer in its earliest stages, at stage 1 or 2, even before symptoms are present.
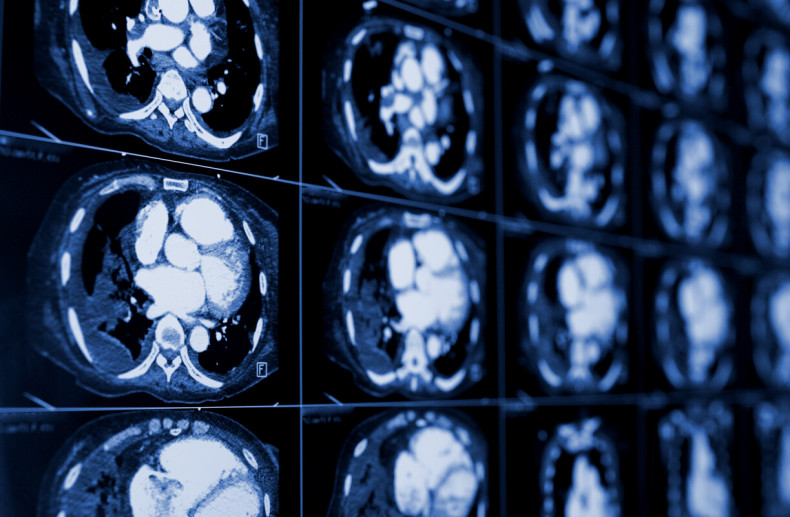
A low-dose CT scan of the chest can help doctors understand if patients have lung cancer.
Experts in minimally invasive procedures
At RB&HH Specialist Care, our experts are dedicated to minimising the impact of surgical and non-surgical interventions on our patients, to improve recovery times and reduce the pain experienced compared to traditional open surgery.
We currently offer two key minimally invasive procedures for lung cancer removal, depending on the type and stage of cancer.
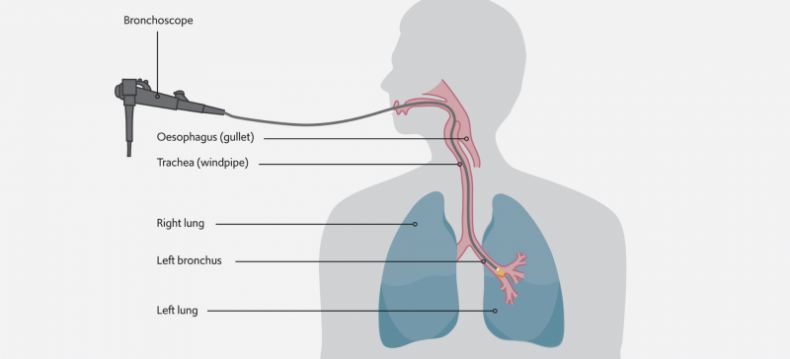
A bronchoscope with a camera at its end is used to access the cancer growth from within the lung’s airways to apply the freezing cryotherapy treatment directly to it.
Endobronchial cryotherapy uses a bronchoscope – a flexible tube-like device with a camera at its end – to reach the part of the airways affected by cancer and apply a cryogen – a substance that produces very cold temperatures between -78°C and -187°C – from its tip directly to the cancer to kill it.
“It is a short minimally invasive procedure lasting around 20 minutes and has been used for over 25 years for the effective treatment of lung cancers blocking the airways. It is a suitable option for patients with advanced lung cancer that cannot be operated on and have few other treatment options available, where it helps them to breathe better,” explains our consultant thoracic surgeon, Mr Nizar Asadi.
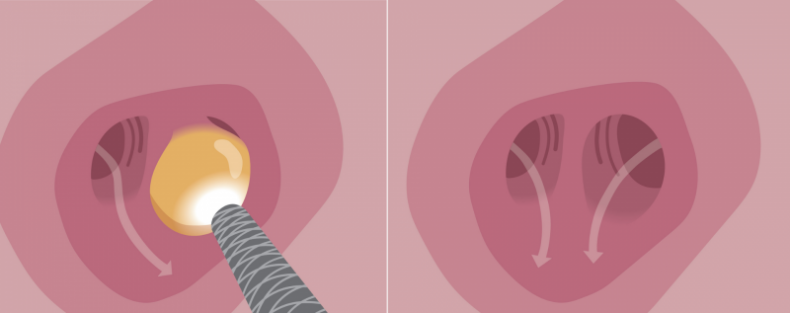
The freezing cryotherapy treatment kills the lung cancer cells which are then naturally removed from the body. After one or more cryotherapy treatments, the growth is completed cleared or reduced in size.
“If we manage to catch lung cancers early enough when they are small and localised to the airways, the treatment can be curative in some patients. Otherwise, it can work to reduce the size of the cancer growth so that less of the lung tissue needs to be removed during a lung resection procedure (a surgical procedure to remove part of the lung with cancer) and so ensuring lung function is preserved as much as possible.”
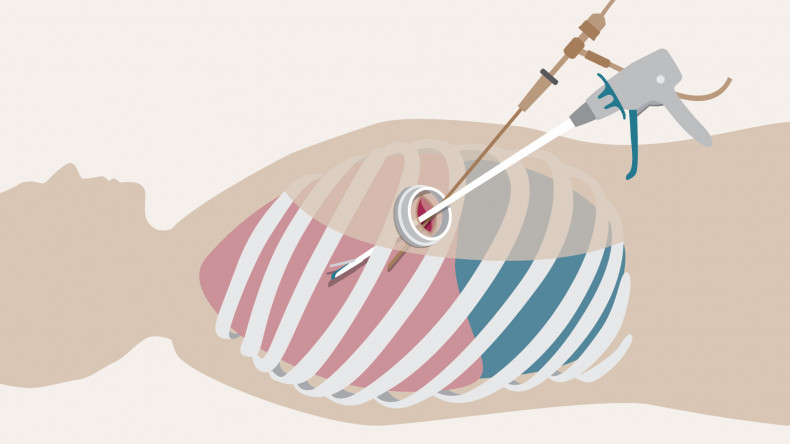
Single-port (also known as single-incision) video-assisted thoracoscopic surgery is a minimally invasive keyhole surgical procedure that can be used to remove lung cancers.
Video-assisted thoracoscopic surgery (VATS) offers lung cancer patients a minimally invasive option to remove parts of the lungs affected by cancer to help prevent the spread of the disease.
Single port (or single incision) VATS offered at our centre, is a keyhole surgery procedure, where a camera and surgical instruments are inserted into the chest via one small incision to navigate to the part of the lung affected, avoiding the need for open thoracotomy (open chest surgery).
“Results from the VIOLET study which involved 503 patients from multiple centres in the UK showed that patients undergoing a VATS procedure experienced significantly less pain, better physical function and fewer complications compared to traditional open lung surgery. They also spent one day less in hospital, on average,” explains Professor Lim, who led the study.
Contact us
For more information or to book an appointment, please contact our customer care team.

