What is aortic regurgitation?
Aortic regurgitation, also known as aortic insufficiency, is a type of heart valve disease – a condition known to affect around 1.5 million people over the age of 65 in the UK.
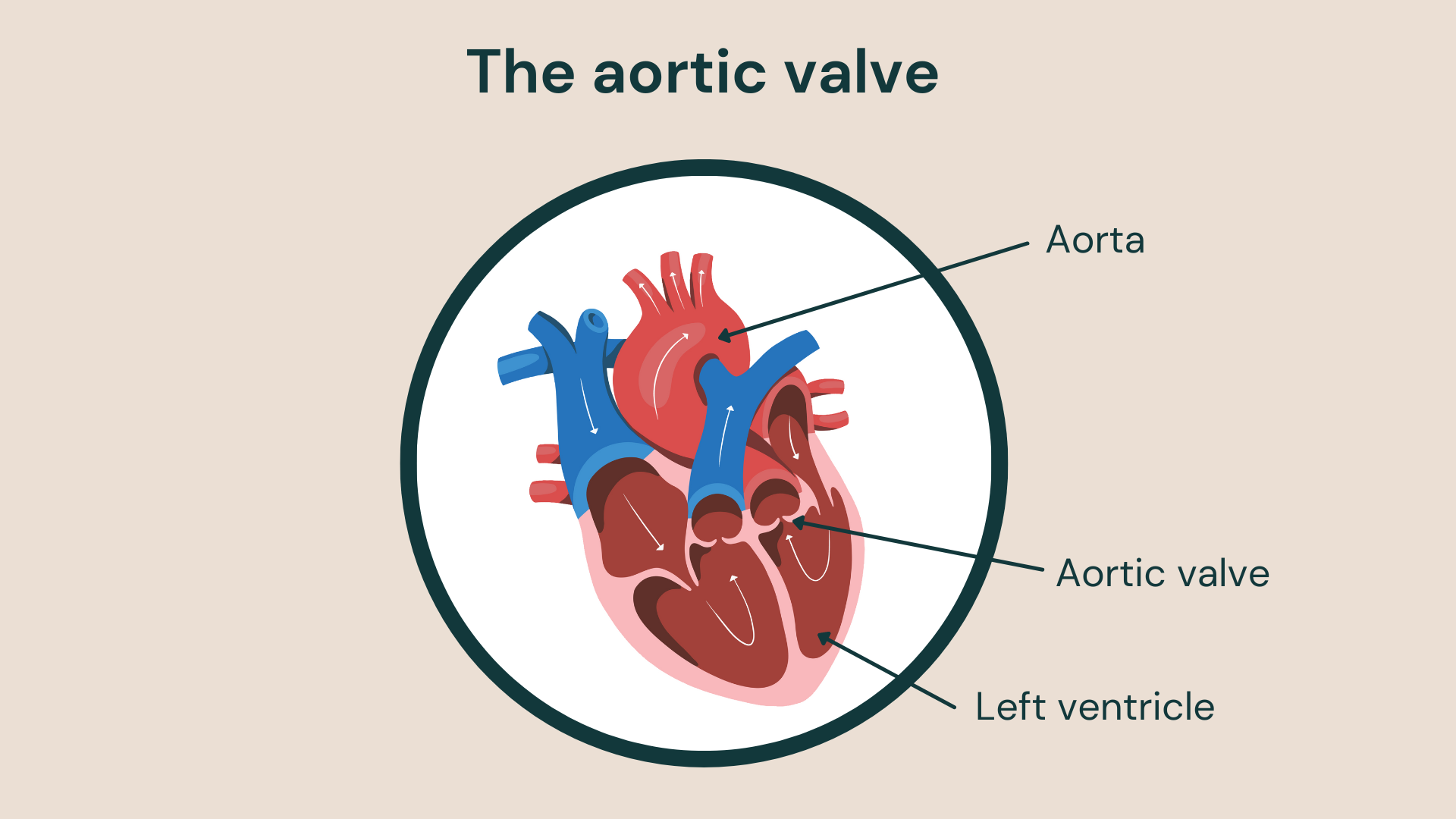
The aortic valve controls the blood flow from the heart to the rest of the body.
The aortic valve controls blood flow from the heart to the rest of the body. During aortic regurgitation, the flaps of the aortic valve don’t close properly, causing blood to leak back into the left ventricle (left lower chamber of the heart) and putting added strain onto the heart.
Over time, aortic regurgitation can lead to your heart becoming weakened and enlarged, due to the extra work the left ventricle has to do to push blood through the leaky aortic valve.
Aortic regurgitation symptoms
Aortic regurgitation usually develops gradually. In fact, you probably won’t experience any aortic regurgitation symptoms for many years, so you may not even realise that you have it.
The condition can be brought on suddenly if due to aortic valve infection.
As regurgitation starts to worsen, you may experience symptoms like:
- fatigue – especially when exercising
- weakness – especially when exercising
- shortness of breath – when exercising or lying down
- arrhythmia – an irregular heart rhythm
- heart palpitations – a fluttering, rapid heartbeat
- chest pain or tightness – which can increase with exercise
- dizziness or fainting – you could feel lightheaded or even lose
- consciousness when exercising
- swollen ankles and feet – due to disturbed blood flow
If you notice any symptoms or signs of aortic regurgitation, contact your doctor immediately. The first symptoms of the condition – such as shortness of breath, fatigue and swollen ankles or feet – could be related to heart failure.
What causes aortic regurgitation?
The aortic valve is one of the heart’s four valves. It separates the left ventricle (the heart’s main pumping chamber) from the aorta (the main artery supplying blood to the body).
Aortic regurgitation happens when the aortic valve doesn’t close properly, causing blood to leak back into the left ventricle and leading to several potential complications.
Some of the main causes of aortic regurgitation typically include:
- congenital heart valve disease – some people have an abnormal aortic valve present from birth which can make you more likely to develop aortic regurgitation
- aortic stenosis – this condition is caused by the narrowing of the aortic valve which can block or stop the valve from closing properly
- rheumatic fever – a result of bacterial infection known as strep throat which can result in a narrow and stiff aortic valve
- endocarditis – inflammation of the lining of the heart chambers and valves may damage the aortic valve
- trauma or tear of the aorta – a chest injury or dissection could result in the backward flow of blood through the valve
- rare conditions – diseases like the inherited connective tissue disorder Marfan syndrome and other autoimmune conditions can cause aortic regurgitation
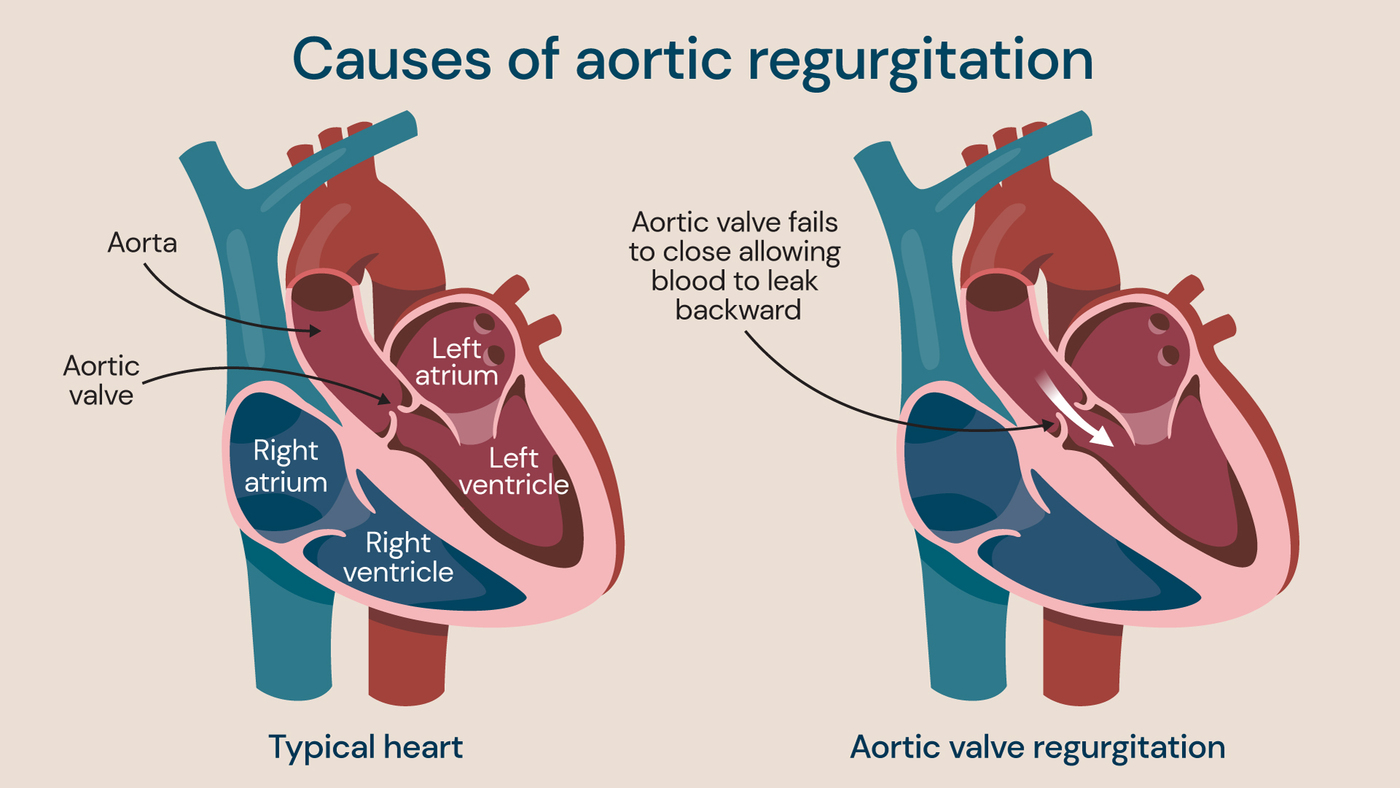
Aortic regurgitation occurs when the aortic valve doesn’t close properly and allows blood to leak back into the left ventricle.
Risk factors for aortic regurgitation
You may be more likely to develop aortic regurgitation if you:
- are an older person
- have previously had an infection that may affect the heart
- have a congenital heart condition (a heart condition present at birth)
- have another type of heart valve condition
- have a specific condition that can cause aortic regurgitation (such as Marfan syndrome and some autoimmune disorders)
- have high blood pressure
Complications of aortic regurgitation
There are several potential complications of aortic regurgitation, particularly if the condition is not treated. These typically include:
- dizziness
- fainting
- infections affecting the heart, such as endocarditis
- arrhythmias (heart rhythm problems)
- heart failure and death (in severe cases)
Diagnosing aortic regurgitation
To diagnose aortic regurgitation, a doctor would initially perform a physical exam using a stethoscope, checking for signs such as heart murmurs. During this initial assessment, you will also usually be asked about your symptoms and your family’s medical history.
There are a range of tests available to help diagnose aortic regurgitation. These include:
- echocardiogram – used to create images of the heart, look closely at the condition of the aortic valve and aorta using sound waves
- electrocardiogram (ECG) – used to measure the heart’s electrical activity to detect signs of heart disease and arrhythmias
- cardiac MRI – used to provide detailed pictures of the aortic valve and aorta using magnetic resonance imaging (MRI)
- chest X-ray – used to show if the aorta or heart is enlarged, and help assess your lung condition
- stress test – used while exercising (or using medication to simulate exercise) to determine aortic regurgitation severity
- cardiac catheterisation – used to diagnose aortic regurgitation when other tests haven’t been able to determine the full diagnosis or level of severity. The test involves using a catheter (long, hollow tube) to inject a dye that can enhance X-ray images
Aortic regurgitation treatment
Treatment for aortic regurgitation will depend on the underlying cause and severity. If you aren’t experiencing any symptoms, your doctor may monitor your condition with regular follow-up appointments and recommend healthier lifestyle changes like losing weight, following a healthy diet and cutting down on alcohol.
The treatment options for aortic regurgitation include:
- medications – including drugs to lower blood pressure, calcium channel blockers and diuretics (to help prevent fluid build-up)
- aortic valve repair – including a variety of procedures to either reshape the valve flaps, patch holes in the valve, remove excess valve tissue or separate valve flaps that are fused together. Leaking replacement valves may also be repaired by inserting a plug using a catheter
- aortic valve replacement – to remove the damaged valve and replace it with a mechanical valve (made from an artificial material such as metal or carbon) or biological tissue valve (made from human or animal heart tissue). This can be done using open surgery or a minimally invasive technique via smaller cuts. In very selected cases a transcatheter aortic valve replacement (TAVR) can be considered
Locations
Diagnosis and treatment for aortic regurgitation is available at the following locations:
Discover our team of cardiology experts
Meet our team of leading cardiologists and cardiac surgeons. From heart health to advanced interventions, our specialists are here to provide personalised care to you
