What is atrial fibrillation?
Atrial fibrillation is a heart rhythm disorder that causes your heartbeat to be irregular, either too fast or too slow. It is the most common irregular heart rhythm disorder (arrhythmia) in the UK, affecting approximately 1 in 45 people.
Older adults are at the highest risk for atrial fibrillation, as it can often occur due to age-related changes in the heart. However, people of any age can experience atrial fibrillation; younger adults and children may, in extremely rare cases, develop the condition due to genetic predisposition or other underlying health conditions.
If you are diagnosed with atrial fibrillation, your risk of stroke can increase by up to 5 times. However, your doctor can prescribe blood-thinning medications to greatly reduce your risk.
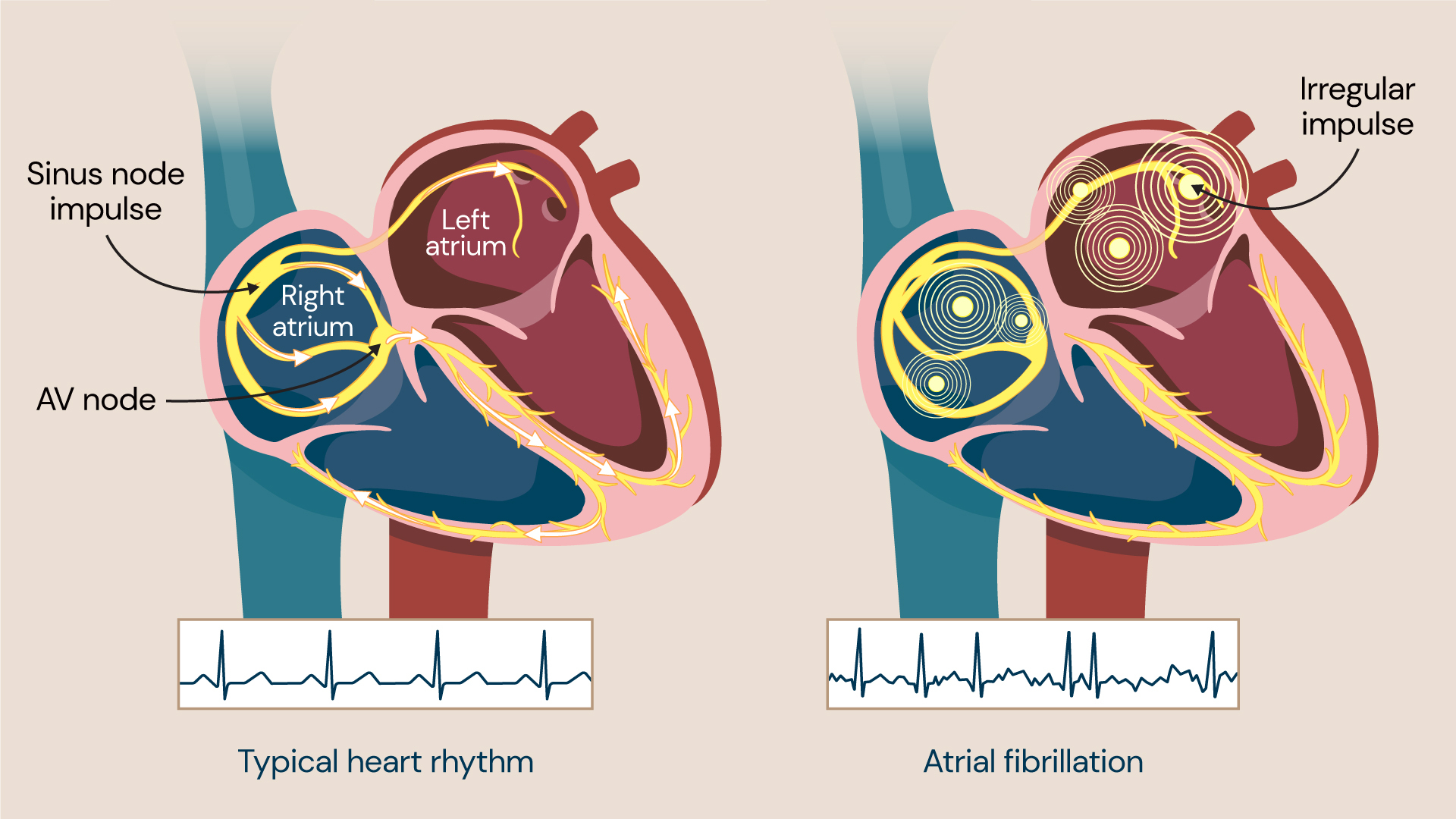
When you have atrial fibrillation, the atria (upper chambers of the heart) beat irregularly and out of sync with the ventricles (lower chambers of the heart). For this reason, atrial fibrillation can cause symptoms such as heart palpitations (a rapid, pounding heartbeat), shortness of breath, and fatigue.
While the condition itself usually isn’t life-threatening, it will require treatment to prevent any serious complications.
Atrial fibrillation occurs when the heart rhythm is irregular and either beats too fast or too slow. It is the most common arrhythmia.
Atrial fibrillation symptoms
You might not experience any symptoms if you have atrial fibrillation. This is one of the main reasons why many people have it and yet remain undiagnosed – approximately 0.5% of the world’s population are currently living with undiagnosed atrial fibrillation.
Typical symptoms of atrial fibrillation often include:
- tiredness – due to the heart not pumping sufficient oxygenated blood to the rest of the body
- weakness – a result of the heart’s inefficiency caused by atrial fibrillation
- breathlessness – during exercise, everyday activities, or even at rest
- palpitations – an awareness of your heart beating abnormally (too fast, too slow or irregularly, for example).
- a heart rate that is consistently lower than 60 or above 100 beats per minute
- reduced ability to exercise – the irregularity of the heartbeat can make exercising difficult
- chest discomfort – pain, pressure, or tightness in the chest
- dizziness – when your heart beats more quickly than normal, your blood pressure can drop, and you may start to feel faint
Symptoms of atrial fibrillation are often classified by how long they last:
- occasional symptoms come and go, may last for anything from a few minutes to several hours or days, could go away on their own, and may need treatment
- persistent symptoms don’t go away on their own, and medications may be required to restore and retain a normal heart rhythm
- long-standing persistent atrial fibrillation symptoms are continuous and last for longer than a year
- permanent atrial fibrillation symptoms mean that a regular heart rhythm cannot be restored and that medications are required to prevent blood clots and control your heart rate
You should see your doctor if you experience any of the above symptoms.
What causes atrial fibrillation?
The heart is made up of chambers surrounded by muscular walls. There are two chambers at the bottom of the heart, called ventricles, and two at the top, called atria.
When the heart beats normally, the muscular walls of the atria and ventricles tighten and contract in turn, to push blood out of the heart and around the body. The muscular walls then relax to allow blood to fill the heart.
When you have atrial fibrillation, the atria (upper chambers) contract randomly and sometimes faster than normal. This means that your heart muscles can’t relax properly, reducing how effectively your heart can work.
Atrial fibrillation occurs as a result of abnormal electrical impulses in your heart. When these start firing randomly in the atria, this overrides your heart’s natural pacemaker, causing an irregular heart rhythm and pulse rate.
The exact cause of these abnormal electrical impulses remains unknown. However, research shows that the chances of having the condition increase with age, typically affecting people aged over 65 most commonly.
Atrial fibrillation risk factors
Atrial fibrillation has several risk factors. These include:
- age – the older you are, the more risk you have of developing the condition
- diabetes
- drinking alcohol – especially binge drinking, which can be a trigger for some people
- high blood pressure
- obesity
You are also more likely to have atrial fibrillation if you have certain other medical conditions, such as:
- atherosclerosis (narrow arteries due to a build-up of fatty deposits)
- diabetes
- heart disease
- heart valve problems
- high blood pressure
- kidney disease
- lung disease
- metabolic syndrome (a combination of diabetes, high blood pressure and obesity)
- sleep apnoea (when breathing stops and starts in your sleep)
- thyroid disease
Complications of atrial fibrillation
Atrial fibrillation can cause complications, especially if the condition is not treated.
Atrial fibrillation’s chaotic heart rhythm can result in blood collection in the atria (upper heart chambers), forming blood clots. Blood clots in the left atrium (left upper chamber) can break free and travel to the brain, which can then cause a stroke.
You are also more likely to have a stroke from atrial fibrillation if you are older, have diabetes, have high blood pressure, have heart failure, or have a valvular disease (a disease involving one or more of the heart’s four valves).
Diagnosing atrial fibrillation
There are several tests available to diagnose atrial fibrillation. Initially, your doctor may examine you and ask various questions about your symptoms and medical history.
Standard tests that can help diagnose the condition include:
- electrocardiogram (ECG) – an ECG detects whether your heart rhythm and its electrical activity (that stimulates heartbeats) is normal. It’s a pain-free test which takes approximately 5 minutes. Small stickers called electrodes will be attached to your chest, arms and legs during the test. These connect to the ECG machine using wires and record your heart’s electrical activity
- echocardiogram – this is an ultrasound scan of your heart. An ultrasound is a procedure that uses high-frequency sound waves to develop a picture of your heart. It is used to check the structure of your heart and its valves, and whether it functions correctly
- chest X-ray – sometimes, lung problems may cause atrial fibrillation. An X-ray of your chest may be used to check if that is the case
- blood tests – a range of blood tests can be used to determine underlying health conditions that may be behind the symptoms you are experiencing
- Holter monitor – a portable ECG device worn on your belt or carried in a pocket or shoulder strap. It can monitor your heart continuously during daily activities over a 24-hour to 7-day period
- event recorder – a carriable monitor worn for much longer than a Holter monitor (usually 2 weeks). The wearer presses a button whenever they start to feel symptoms
- exercise stress test – this is a test done during exercise (or using a medication that mimics exercise) that can show how well your heart is working
Atrial fibrillation treatment
Treatment for atrial fibrillation will depend on the underlying cause and severity. However, the key treatment options available are detailed below.
Medications
Your doctor can prescribe blood-thinning medications called anticoagulants to help reduce your risk of a stroke, which is common with atrial fibrillation.
They may also prescribe medications to help control your heart rate and return it to normal. These might include:
- anti-arrhythmic medications
- beta-blockers
- calcium channel blockers
Cardioversion therapy
Cardioversion therapy is a procedure that involves shocking your heart to help return its rhythm to normal. It is typically carried out in a hospital to allow your healthcare team to keep a close eye on your heart until they feel it’s safe for you to return home.
The procedure can be done using 2 key methods:
- Electrical cardioversion, which resets your heart rhythm by sending electrical shocks to the heart through electrodes.
- Drug cardioversion, which uses medications administered intravenously to reset your heart rhythm.
Catheter ablation
Catheter ablation involves very carefully destroying the diseased area of your heart that is responsible for irregular electrical activity. It’s typically recommended if medication hasn’t worked for you or if you can’t tolerate it.
During the procedure, a catheter – a soft, thin wire – will be guided through one of your veins to your heart, where it will be used to record electrical activity. Once the source of the abnormal electrical activity in your heart has been identified, a high-frequency radio wave will heat the diseased part of your heart and destroy the tissue.
The whole procedure usually takes between 2 and 3 hours to complete, so you may be put to sleep using a general anaesthetic while it takes place. However, you should recover quickly and be able to carry out most of your normal activities the very next day.
Pulse field ablation
Pulse field ablation (PFA) is an innovative medical procedure for treating atrial fibrillation. It’s an advanced form of catheter ablation that uses high-voltage electrical pulses to destroy abnormal heart cells that cause irregular electrical signals. This allows the heart to resume its normal rhythm.
PFA is more tissue-selective than other more established ablation techniques. This means that it targets the heart muscle cells directly without affecting the surrounding structures. PFA does not use thermal (heat) energy, resulting in a lower risk of complications such as oesophageal injury, nerve damage, and blood clots.
The procedure begins with inserting a catheter guided to your heart and positioned near the pulmonary veins. This is often where abnormal electrical signals originate, triggering atrial fibrillation.
The electrophysiologist performing the PFA procedure then maps your heart’s electrical activity to pinpoint the specific area that requires treatment. Then, high-voltage electrical pulses are delivered to the heart tissue, destroying the faulty cells.
Although PFA is relatively new, it’s an exciting advancement in treating atrial fibrillation, and it could become a widely adopted technique.
Pacemaker
Pacemakers are usually used to stop your heart from beating too slowly. Still, they can also be used in cases of atrial fibrillation, where the heart tends to beat too slowly, or in combination with a procedure that disconnects the top chambers from the heart’s bottom chambers.
A pacemaker is a small battery-operated device implanted surgically in your chest, just below your collarbone. Inserting it will involve a minor surgical procedure that can be carried out with local anaesthetic (numbing the area to be operated on) whilst you are awake.
Inserting a pacemaker is often recommended if your heart is no longer responding to medications or if they are unsuitable for you to take. This is most common in people aged over 80, but younger adults can also have pacemakers implanted if required.
Pacemakers can be used to help the heart beat more regularly.
How to prevent atrial fibrillation
Leading a healthy lifestyle can reduce the risk of heart disease and help prevent atrial fibrillation. Here are some top tips for maintaining a healthy heart:
- quit smoking – lowers the risk of atherosclerosis (fat deposits in the arteries) and blood clots
- exercise often – helps to prevent high blood pressure and maintain a healthy weight
- eat a low-fat, low-salt diet – prepare meals rich in fruit, vegetables, and whole grains
- manage stress – when you are stressed out or angry, heart rhythm problems can occur
- limit alcohol or caffeine intake – or avoid them entirely
Locations
Discover our cardiology experts
Meet our team of cardiologists specialising in atrial fibrillation. Whether you need help maintaining heart health or implementing innovative interventions, our experts are here to offer personalised care tailored to your needs.
