Pacemakers and implantable cardioverter defibrillators (ICDs) are different types of implanted electronic devices that treat slow, abnormal and dangerous heart rhythms and help your heart function.
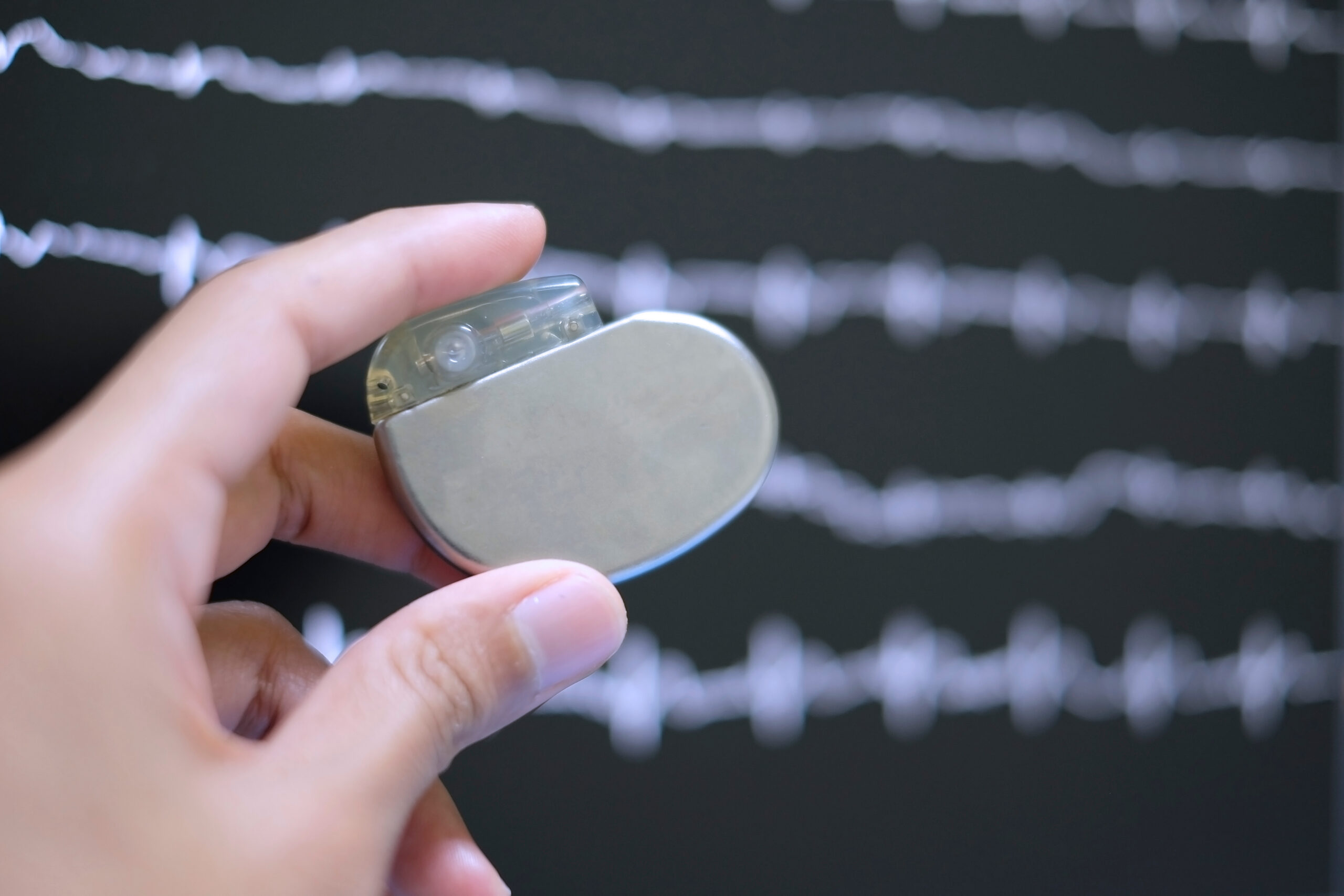
Pacemakers and ICDs are small battery-powered devices. They are normally sited beneath the superficial fat layer just below the collarbone. They are connected to the heart through fine leads, which work to monitor the heart’s electrical activity and transmit electrical impulses to regulate the heartbeat.
What controls the heartbeat?
Your heart has an electrical system that controls the heartbeat. The heart’s rhythm and rate are regulated by the sinus node, which functions as the heart’s inbuilt natural pacemaker. In a healthy heart, the node sends regular electrical impulses to the cardiac muscles, making them contract and pump blood.
If the sinus node is faulty, or there is a problem with the conducting tissue between the top and bottom chambers of the heart then the heart may beat abnormally slowly. In these circumstances, pacemaker implantation is required to prevent the heart from going too slowly which may cause dizzy spells or excessive fatigue. In cases where the heart muscle has become damaged due to heart attacks or diseases of the heart muscle (cardiomyopathy), the heart can go into a dangerously fast heart rhythm. In these circumstances, your cardiologist may recommend that you have an ICD implanted.
What is a pacemaker?
A pacemaker is an electronic device implanted in your body to treat slow or abnormal heart rhythms and support your cardiac function.
You may need a pacemaker if you have a slow or irregular heartbeat. A pacemaker can work on-demand or all the time to regulate your heart rate and help your heart work effectively.
Special types of pacemakers called biventricular pacemakers or cardiac resynchronisation therapy (CRT) can also coordinate the way your heart chambers contract. These devices may help improve heart function and treat heart failure.
You may need a pacemaker if you have a slow or irregular heartbeat.
What is an ICD?
ICD stands for implantable cardioverter-defibrillator. ICDs are small electronic devices that can be implanted in your body. An ICD transmits electrical pulses which regulate abnormal and dangerous heart rhythms.
You may need an ICD if your heart has gone into an abnormally fast heart rhythm disturbance or if your heart has been damaged by previous heart attacks or heart muscle disease (cardiomyopathy). if you are at risk of dangerous heart rhythms that could cause sudden death.
What does a pacemaker do?
A pacemaker takes over the work of a faulty sinus node. It consists of a small box containing a battery and an electric circuit, and electrode leads. The battery sends regular electrical impulses through the leads to your heart muscles. Each impulse makes the heart muscle contract and produces a heartbeat.
A pacemaker continuously monitors your heart’s electrical activity. It can work constantly (called fixed-rate pacing) or on-demand when your heart beats too slowly or skips beats. Some devices can also work to increase your heart rate when you’re exercising to meet your body’s increased needs.
A biventricular pacemaker is a special kind of device that helps synchronise the heart chambers’ contraction, improving the pumping action and treating heart failure.
What does an ICD do?
An ICD works to control and regulate your heartbeat. It consists of a small box containing a battery-powered electric circuit and electrode leads that connect it to your heart.
An ICD continuously monitors your heart’s rate and rhythm. If it detects a dangerous arrhythmia, it can act in three ways to restore a normal rhythm:
Pacing: An ICD can act as a pacemaker, taking over the function of the heart’s natural pacemaker or conducting tissue. The device can send electrical signals through the leads to the heart muscles. Each impulse makes the heart contract and produces a heartbeat.
Antitachycardia pacing (ATP): If the ICD detects that the heart has gone into an abnormally fast, life-threatening rhythm disturbance it will pace the bottom chambers of the heart to try to terminate the rhythm disturbance. you may not be aware of this happening. The ICD can transmit small low-energy electric shocks to restore a normal rhythm if it has become irregular.
Defibrillation: In circumstances where the ICD detects that the heart has gone into an abnormally fast rhythm disturbance and that your life is in danger it will deliver a small electric shock which will terminate the rhythm disturbance. The ICD can administer larger electric shocks to treat dangerous potentially fatal arrhythmias and restore the heart’s normal rhythm.
How are pacemakers and ICDs fitted?
Pacemakers and ICDs are usually implanted in a minimally invasive procedure in a cardiac catheterisation laboratory or ‘cath lab’. However, if you are having open-heart surgery for another problem, the cardiothoracic surgeon may implant the device simultaneously.
Your specialist will usually administer a local anaesthetic to numb the area and sedation to keep you relaxed throughout the procedure. You may feel some pressure and pulling, but it shouldn’t be painful.
Your cardiologist will make a small incision in the skin under your left collarbone. They will insert fine leads into a blood vessel and guide them into your heart using X-ray guidance. When the leads are in the correct position, the specialist will connect them to the pacemaker or ICD box. They will check the device is working properly, monitoring the heart’s electrical activity and providing the right stimulation level.
Your specialist will make a space known as a ‘pocket’ under the skin below your collarbone to hold the box. Finally, they will use stitches or medical glue to close the incision and apply a dressing. ICDs and pacemakers are slim, and around the size of a matchbox, so they are usually pretty well covered by the tissue on the chest wall, although they can be more evident if you are very slim.
ICDs and pacemakers are often fitted as a day case. However, your cardiology team may keep you in the hospital overnight or longer to closely monitor your recovery.
More information
Who can benefit from a pacemaker?
You will need a pacemaker if there are problems with your heart’s conduction system or its ability to pump blood effectively. You may notice that your heart rate is slow, experience palpitations, or feel that your heart pauses or skips a beat. Problems with the heart’s rhythm or function cause chest pain, breathlessness, and ankle swelling and may make you feel faint and exhausted.
You may need a pacemaker if you have:
- bradycardia (a slow heartbeat)
- heart failure
- sick sinus syndrome: problems with your heart’s natural pacemaker doesn’t work correctly
- heart block-a delay or interruption to the electrical impulses between the upper and lower heart chambers, which slows the heartbeat
- atrial fibrillation: If atrial fibrillation is making your heartbeat too slow, a pacemaker can help. If the beat is fast and irregular, you will need other treatments like medication
- cardioinhibitory syncope: fainting or collapse because of a pause in the heartbeats
See your doctor or make an appointment with a specialist cardiologist if you are worried about your heart health.
Who can benefit from an ICD?
You might need an ICD if you are at risk of potentially life-threatening heart arrhythmias that could cause sudden death. You may have already had an abnormal heart rhythm, or tests may have confirmed that your heart has been damaged because of previous heart attacks or cardiomyopathy. ICDS are also implanted in patients who have inherited abnormalities of the ion channels within the heart cells. show that you’re at risk of an arrhythmia in the future because of faulty genes or heart disease.
You may need an ICD if you have:
- had either ventricular tachycardia or ventricular fibrillation in the past
- survived a sudden cardiac arrest in the past
- cardiomyopathy
- long QT syndrome
- Brugada syndrome
- heart failure which could cause a dangerous arrhythmia
- inherited electrical abnormalities of the heart (often there is a family history of unexplained sudden cardiac death)
Fixed price packages for self-funders
If you prefer to pay for your own inpatient treatment, we offer fixed-price packages to help manage the cost of surgery and care while in the hospital.
As the treatment needs vary from patient to patient, you will need to provide an up-to-date medical report or referral to be reviewed by the agreed consultant.
A complimentary consultation to review this report and any test results you have can be arranged. This will determine whether you are eligible for our fixed package price.
For more information regarding our fixed-price packages, please contact our customer care team.
Locations
Our specialists can see patients in the following locations:
Discover our dedicated cardiology specialists
Meet our team of renowned cardiology specialists. From cardiovascular health assessments to innovative interventions, our experts are committed to delivering personalised care designed just for you.
