What is retinal detachment?
A retinal detachment occurs when your retina separates from the inside of your eye. The retina is made up of layers of nerve tissue at the back of your eye. It receives images and sends visual signals through the optic nerve to the brain, which is how you process what’s in front of you to turn it into an image to see.
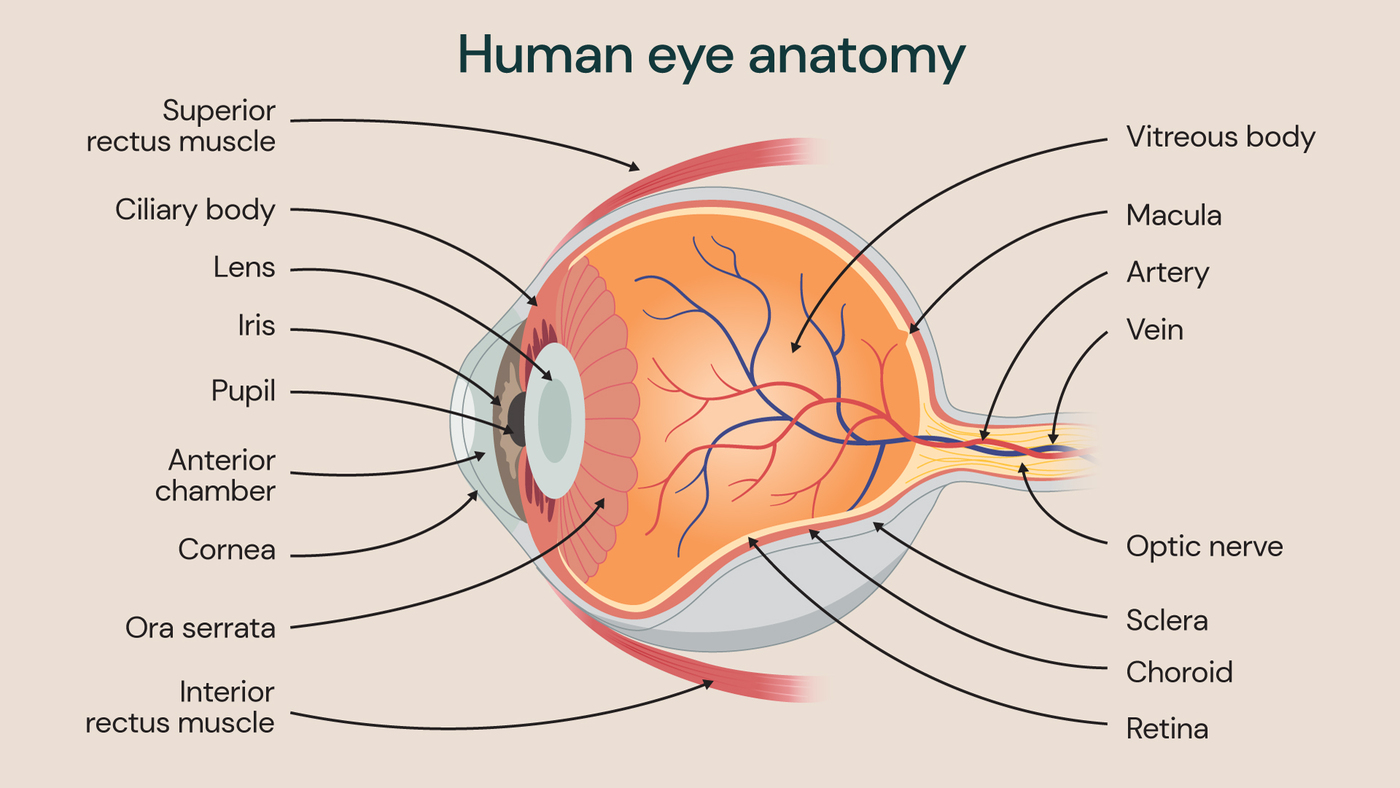
Illustration showing the anatomy of the human eye.
The eye is filled with a fluid called the vitreous humour. It’s a jelly-like substance that fills the area behind the eye’s lens and in front of the retina, consisting of collagen, fluid and various nutrients. Problems with the vitreous humour can lead to an increase in floaters (dots or lines appearing in your vision) and, if the vitreous humour pulls too much on the retina, it can cause the retina to detach.
Retinal detachments are most common in people aged 40 to 70 years old and affect 10-15 per 100,000 people each year. This makes retinal detachment one of the most common eye emergencies in the UK. Professor Roger Shimizu Wong, consultant vitreo retinal and ophthalmic surgeon at St Thomas’ Hospital, explains more about retinal detachments, and how you can identify one.
What are the different types of retinal detachment?
There are 3 different types of retinal detachment, each of which is caused by something different.
Retinal holes and tears
This is the most common cause of retinal detachment, with a tear or hole in the retina allowing fluid to leak between the layers of the retina. This fluid causes the retina to lift away from the back of the eye and detach. With age, it’s also common for the eye’s vitreous gel to come away from the retina and, with it, pull on the retina causing a tear.
Scar tissue
Some people may develop scar tissue on the surface of their retina due to conditions such as diabetic retinopathy, trauma or infections and inflammation within the eye. The scar tissue can cause puckering and pull on the retina, leading to detachment.
Fluid leaking
The rarest cause of a retinal detachment occurs when the blood vessels behind the retina leak fluid between the different layers of the retina. There are no holes or tears with this type of retinal detachment, but the leaking occurs due to eye inflammation or tumours.
What causes retinal detachment?
The most common causes of retinal detachment are age and trauma directly to the eye. With age, the vitreous humour can change and shrink, pulling on the retina, therefore causing the retina to tear and peel away from the back of the eye. This process is called posterior vitreous detachment (PVD). The retinal detachment itself is painless, although the visual changes and symptoms that come with it are worrying and need treatment as soon as possible.
“There is some link to a family history of retinal detachments increasing your likelihood of having one, although it’s rare that this would be the cause over ageing or an eye injury,” explains Professor Wong.
What increases your risk of retinal detachment?
There are several factors that can increase your risk of a retinal detachment, including if:
- you are short-sighted (struggle to see objects in the distance)
- you have recently had an eye operation, such as cataract surgery
- you have had a retinal detachment in one eye previously
- you have a family history of retinal detachment
What does retinal detachment look like?
There are several visual symptoms that suggest you may be experiencing retinal detachment. One of the key indicators is a sudden increase in the number of floaters you see in your vision. “Floaters can appear as dots or squiggly lines, and it’s important to know that it’s normal to have some of these,” says Professor Wong. “However, your floaters should be stable, and any sudden increase or change should be checked promptly by a specialist.”
A second symptom of retinal detachment is flashes of light in your vision. These flashes can last anywhere from just a split second to up to a few seconds. It occurs when the vitreous gel inside the eye shrinks or changes in shape, and then pulls on the retina. It’s this pulling that can cause the retina to detach so, if you experience this symptom, seek medical advice quickly.
“If you notice a dark shadow or a ‘curtain’ type movement across your vision, this is another sign of retinal detachment which shouldn’t be ignored,” explains Professor Wong. It typically begins in your peripheral vision and then grows in size, covering your field of vision. Unlike the flashes which can come and go, the dark shadow associated with retinal detachment will stay and worsen until you seek urgent treatment.
A final visual symptom of retinal detachment is a sudden blurring in one eye. “Blurring in both eyes might indicate a neurological problem, but blurring in one eye, particularly if it comes on suddenly, can suggest a bleed which can then develop into a retinal detachment,” says Professor Wong. This is because tiny blood vessels in the eye bleed into the vitreous humour, causing clouding of vision.
How long before retinal detachment can lead to blindness?
The amount of time from the first symptoms of retinal detachment to loss of vision varies between individuals, ranging from several hours to a few days.
“The longer the detachment is left untreated, the greater the risk of permanent vision loss is,” warns Professor Wong. “Depending on the extent of the retinal detachment, you should ideally have treatment within 48 hours of your symptoms appearing for the best chance of preserving your vision.”
What happens in vitrectomy surgery to treat retinal detachments?
Vitrectomy is a procedure to repair retinal detachment, which is needed to preserve your vision once you experience symptoms of retinal detachment. The procedure is usually performed on an outpatient basis and you should be free to go home on the same day.
You can have the procedure either under general anaesthetic (where you’re asleep for the whole procedure) or under local anaesthetic (which freezes the area around your eye so you’re awake but feel no pain).
During the procedure, the consultant ophthalmologist carefully removes the vitreous jelly from inside your eye, creating space to insert bubble of gas or silicone oil. The bubble pushes the retina against the back of your eye again, allowing it to heal in place. Depending on the type of gas used, the bubble absorbs itself over 10-14 days, or 6-8 weeks. Your consultant will advise which type is your best option.
Recovery from vitrectomy surgery
After vitrectomy surgery, you may experience grittiness and redness in your eye, and some blurriness in your vision. The symptoms of this should be treatable with paracetamol and should disappear in a few days after your surgery.
You will need to be cleared to drive after your surgery and may need to take time off work if you find your vision is affected by the surgery. However, most people are able to return quickly to their usual daily activities with an uncomplicated recovery period.
Can you prevent retinal detachment?
For retinal detachments caused by age-related changes to the eye, there are no lifestyle changes you can make to prevent them from occurring.
However, when it comes to preventing eye injuries that can lead to retinal detachment, you can invest in protective eyewear for sports or other activities that have a higher risk of leading to eye injuries.
“Above all, the best step you can take to protect your vision is to book regular eye tests with your optician,” says Professor Wong. “This allows you to establish a good baseline of your ‘normal’ vision, and for any early changes that could suggest future eye problems to be detected and treated promptly.”
If you have any concerns about your vision that you would like to discuss with our specialist ophthalmologists at St Thomas’ Hospital, please do get in touch with our team.
Related content
-
Retinal detachment
Retinal detachment is a serious eye condition that requires urgent treatment. Learn more about the symptoms and when to seek treatment from eye specialists.
-
Retinal detachment surgery (vitrectomy)
Vitrectomy is a surgical procedure used to repair retinal detachment.
-
Ophthalmology
Our ophthalmology team offer treatments for visual impairments, eye conditions and diseases.
