Professor Christoph Nienaber’s reputation for being one of the world’s leading interventional cardiologists attracts patients from far and wide. The RB&HH Specialist Care team met with one of his patients, Ruth, to learn about her healthcare journey.
At the age of 83, Ruth had been living a full and active life. A retired cardiologist – internationally recognised in her own right – and a talented and well-respected pianist in her spare time, she had many achievements to be proud of.
However, after taking care of so many others’ hearts during her career, her own started to trouble her. Five years ago, she discovered she had an aortic aneurysm and travelled to Canada soon after from her home in Tel Aviv, Israel, to receive surgery to repair the aorta just above the valve. She recovered well, returning to her retirement and family life. She explains, “Things were very good after that.”
“But, a little over a year ago I was in trouble again; I suddenly had severe back pain which was diagnosed as a new dissection of the thoracic aorta,” Ruth continues. For this, she received a stent at the Rabin Medical Centre in Israel – where she used to work. Again, things seemed to go back to normal after that – until another dissection developed below the stent soon after, weakening the aorta even further.
Ruth explained that as it was considered a relatively small leak and given her age, her local doctors wanted to be conservative with her treatment, suggesting a ‘watch and wait’ approach before exploring any major open, invasive surgery.
However, for Ruth, simply waiting to see what happens was a challenge. “I was active – I’d walk the dog, play the piano, take care of the house a little. And, of course, there were the grandchildren to keep up with. But I was told to restrain my activities.”
“Instead, I decided not to be passive about it and started inquiring about treatment options. I have some very good international friends in the field who I collaborated with in the past. One of them, a famous professor himself, suggested Professor Nienaber. He told me:
“This is a man with a lot of experience. People come from all over the world to be treated by him.”

A personalised care strategy
Professor Nienaber describes first seeing Ruth’s case: “I saw the images that our colleagues in Israel kindly sent over. I found, immediately, that this was a case for a minimally-invasive thoracic endovascular aortic repair (TEVAR) procedure to complete the job – to stop the aorta from further enlargement and possibly rupture. So, we accepted her right away and started to design a personalised non-surgical strategy for Ruth.”
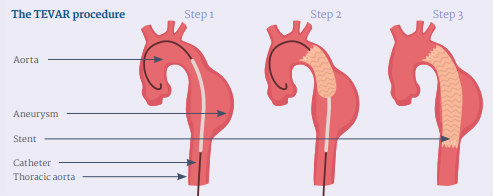
TEVAR is a technique Professor Nienaber helped pioneer over 20 years ago. It only requires a minor incision in the groin to access the area affected in the thoracic aorta, to treat an aneurysm or aortic dissection.
A catheter and guidewire are directed under fluoroscopy to the correct location, where a fabric-covered stent is then precisely launched. This stent seals the aneurysm or covers a leaky wall at the point of dissection.
As for the benefits of TEVAR compared to traditional surgery (opening the chest), Professor Nienaber explains: “The procedure is quick – it only takes between one and three hours and does not require the heart to be stopped. Also, the complication rate and the associated co-morbidity with the TEVAR procedure is much lower than with surgery.
“They usually leave the hospital between three and seven days after. If they are active and working, they go back to work and family life as normal, and without the need for anticoagulants.”
A feeling of ease
“Professor Nienaber is known all over the world, yet he is very approachable and easy to talk to – it’s fantastic. I was very much at ease with him,” Ruth describes of her treatment and care.
Professor Nienaber describes what sets Royal Brompton Hospital apart for TEVAR procedures: “Royal Brompton Hospital has the luxury of a unique hybrid operating room that allows treatment in a sterile environment with optimal imaging capabilities and a conversion option, if you need it, for open surgery.
“We also use a multi-disciplinary approach for these endovascular procedures. There are colleagues from vascular and cardiac surgery, cardiology and radiology in the room to ensure we are prepared for every eventuality.
“Because of this approach, we see excellent results and extremely low morbidity and mortality – much less than that reported in the literature.
“I’m pleased to say that Ruth’s health has returned to normal and she is able to enjoy her hobbies and spend time with her family once more.”
What to look out for in your patient
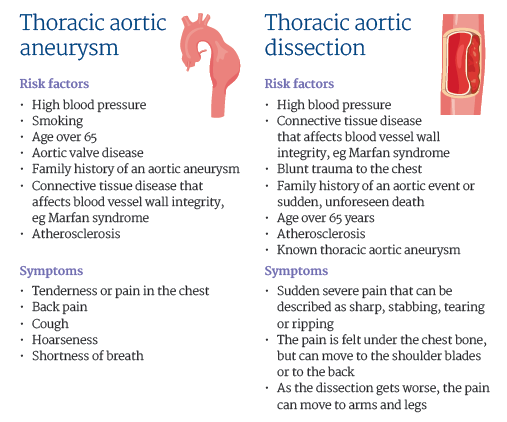
At a glance
Procedure
Thoracic endovascular aortic repair (TEVAR)
Carried out by
Professor Nick Cheshire, head of vascular surgery
Mr Maziar Mireskandari, consultant vascular surgeon
Professor Christoph Nienaber, consultant cardiologist
Mr Ulrich Rosendahl, consultant cardiac surgeon
What problem does it solve?
The TEVAR procedure is used to repair the blood flow following a thoracic aortic aneurysm or dissection.
How does it work?
TEVAR is a minimally-invasive procedure where a catheter and guide wire are inserted through a small incision in the groin. These are directed under fluoroscopy to the location affected in the thoracic aorta (Step 1), where a stent is then precisely placed (Step 2). This covered stent (or endograft) seals the aneurysm or covers a leaky wall at the point of dissection (Step 3).
Contact us
For more information or to book an appointment, please contact our customer care team.
