Microplastics are thought to have started accumulating in the world’s oceans in the 1960s, with the term “microplastics” first coined in 2004 by marine biologist, Professor Richard Thompson. However, it wasn’t until 2022 that the first reports of microplastics in human blood were published. While it’s impossible to know the long-term effects of microplastics in our systems, we’re now starting to see some negative health impacts emerging. Dr Brian Halliday, consultant cardiologist at Royal Brompton Hospital, explores more about the effects of microplastics on the human body.
What are microplastics?
Microplastics are defined as pieces of plastic 5mm or smaller in size. These can either be pieces deliberately manufactured to be tiny, such as glitter or small beads, or occur as a result of larger pieces of plastic breaking down. Microplastics can break off from anything from plastic bottles and Tupperware containers to synthetic clothing fibres released in every clothes wash.
So, how do microplastics enter the human body? Studies have shown that they are in the water we drink and the food we eat, as well as being inhaled from the air and absorbed through the skin. “However, due to the relative recency of awareness of microplastics, and the associated discussions around impacts on human health,” says Dr Halliday, “we don’t know much yet about the long-term effects of living with microplastics in our bodies.”
However, studies from 2019 and 2022 have found that microplastics disrupt hormones, impair immunity, and have negative impacts on the gut microbiome.
Impacts of blocked arteries
A 2024 study found microplastics present in some arterial plaques, and suggested that they may contribute to worse healthcare outcomes.
Coronary artery disease (also known as coronary heart disease) occurs when the coronary arteries that supply the heart with oxygen-rich blood become narrowed. This narrowing happens as a result of fatty deposits (known as plaques) building up in the arteries, blocking the blood flow.
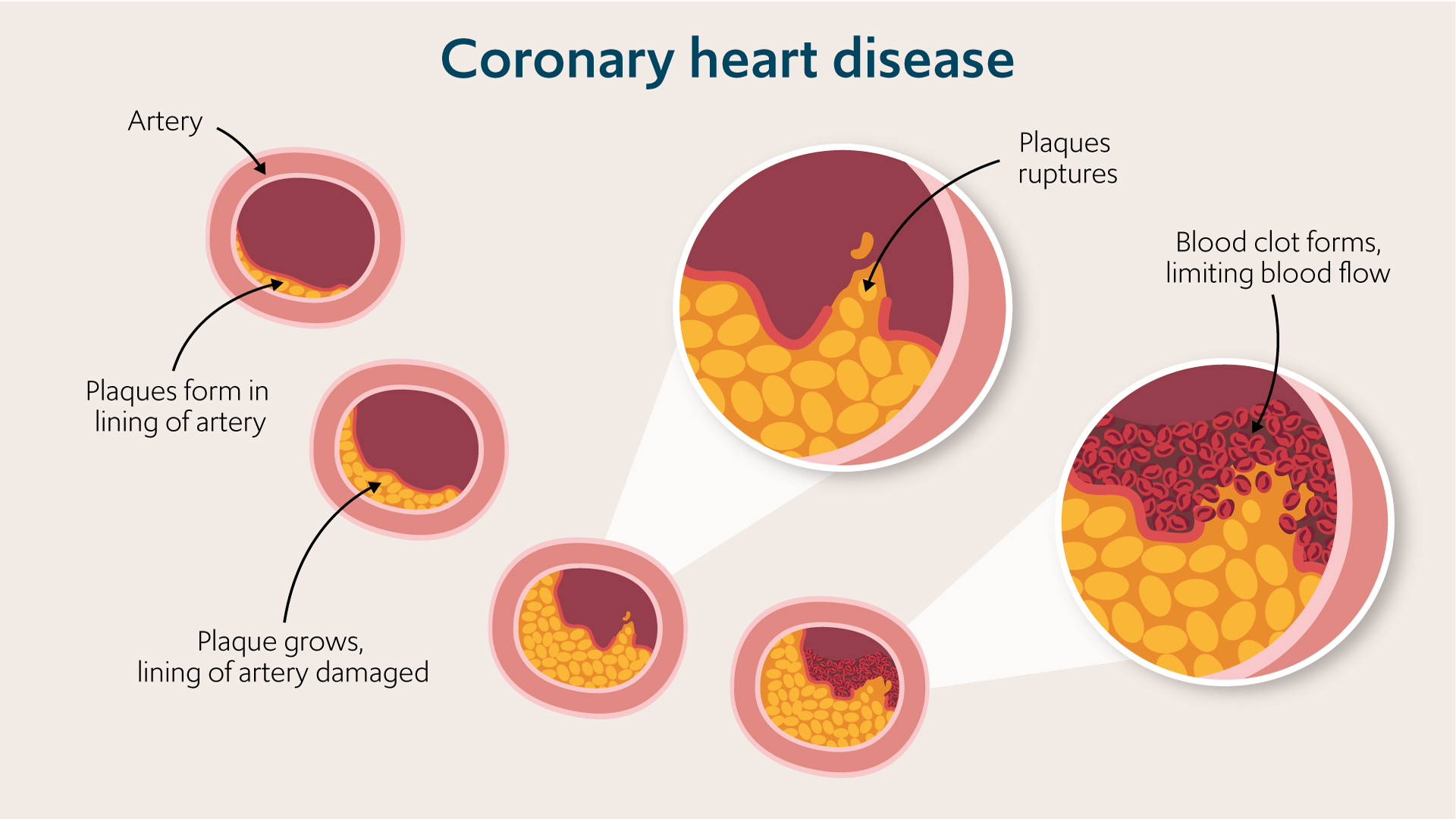
Coronary artery disease is the most common type of heart disease and is the number one cause of heart attacks. Heart attacks lead to around 100,000 hospital admissions in the UK each year, and a build-up of plaque in the arteries is estimated to be the cause of around 50% of all deaths in Europe and North America.
“Coronary artery disease can lead to heart attack or heart failure,” explains Dr Halliday. “Plaque can also build up in the carotid arteries (the main blood vessels which supply blood to the neck, face and brain) which, if left untreated, can also result in stroke.”
Microplastics blocking arterial blood flow
The study, which was published in March 2024, states that microplastics are “emerging as a potential risk factor for cardiovascular disease in preclinical studies.” This is the first study that has observed microplastics in the human body with a link to cardiovascular disease.
The research looked at 304 patients who were undergoing a procedure called carotid endarterectomy. This is a surgical procedure to remove build-up of plaque in the carotid arteries and improve blood flow to the neck, face and – crucially – the brain.
The plaques which were removed from the carotid arteries in the procedures were analysed and microplastics were found in over half of the participants’ samples. 58% of the study’s participants were found to have polyethylene (PE) in their arterial plaques. PE is the most widely used plastic in the world and is present in items we use every day, including plastic water bottles, food containers and bags.
Further to this, 12% of the participants’ arterial plaque samples had plastic polyvinyl chloride (PVC) found in them. PVC is a highly versatile plastic which is used for numerous applications from drainage pipes and window frames to flooring, footwear, packaging and more.
Of the 304 patients in the study, 257 were followed successfully for up to 34 months after their endarterectomy procedures. This follow-up revealed that participants who had microplastics found in their arterial plaques were 4.5 times more likely to have a heart attack or stroke in this period. They were also more likely to die in the 3 years after their plaque removal procedures, compared to the study participants who had no microplastics found in their removed plaques.
Additionally, the plaque that was removed from participants’ carotid arteries was found to be more inflamed when it contained microplastics, compared to the participants who had no evidence of either PE or PVC in their plaque samples.
A build-up of plaque in the arteries is also more common in individuals with diabetes, kidney disease and obesity. However, the authors of the study on microplastics note that “direct evidence that […] risk extends to humans is lacking,” suggesting that further research is required to better understand the dangers posed to the cardiovascular system by microplastics.
They also acknowledge that other behaviours of the patients in the study, including smoking and low activity levels, could have affected the results, rather than linking the outcomes exclusively to the presence of microplastics in arterial plaques.
What are the symptoms of coronary artery disease?
There are several symptoms associated with coronary artery disease. The main indication is angina, which is a tight or heavy sensation of pain, discomfort, tightness or pressure across the front of your chest.
Other symptoms which are indications of coronary artery disease include:
- shortness of breath
- heart palpitations
- rapid heartbeat
- nausea
- sweating
- dizziness
If you experience a combination of these symptoms, it may suggest that you should visit your doctor for a thorough assessment and to discuss your cardiovascular health.
Treatment for coronary artery disease
Coronary artery disease can be managed with the right combination of lifestyle changes, medication and, in serious cases causing symptoms, surgery.
“Recommended lifestyle changes are quite simple and include eating a healthy diet, quitting smoking, and doing more exercise,” says Dr Halliday. “These changes help to reduce the risk of developing fatty deposits in your arteries and the chances that they will lead to complications such as a heart attack.”
Medication is also available and may be prescribed to you if your doctor recommends it. The medication works to reduce blood pressure or widen your arteries, improving blood flow and reducing your risk of complications associated with coronary artery disease.
“Surgical options for treating coronary artery disease may be recommended if you have a severe case of the condition, or if lifestyle changes and medication have not worked to improve your symptoms and health,” explains Dr Halliday. These procedures include coronary angioplasty (minimally-invasive stenting) and coronary artery bypass graft (CABG) which are offered by our cardiology experts to improve blood flow to your heart and minimise the risk of future complications.
Get in touch
Our heart specialists can treat coronary artery disease at Royal Brompton and Harefield hospitals. Contact our team to learn more or to make an appointment with a specialist.
Related content
-
Coronary heart disease
Coronary heart disease is caused by the narrowing of the coronary arteries that supply the heart muscle with oxygen-rich blood.
-
Coronary angioplasty
Coronary angioplasty is a procedure that improves blood flow to your heart.
-
Coronary artery bypass grafting (CABG)
CABG bypasses the narrowed sections of your arteries to improve blood flow.
