For some women, blood sugar levels can become higher than usual during pregnancy. This is called gestational diabetes, or diabetes during pregnancy.
Gestational diabetes isn’t completely preventable — some women will develop the condition no matter how healthy their lifestyle is — but there are ways to help lower your risk of diabetes developing during your pregnancy.
Here’s what you need to know about how to avoid gestational diabetes.
What is gestational diabetes?
Gestational diabetes is a specific type of diabetes that occurs during pregnancy. Studies estimate around 1 in 20 women are affected by this condition.
Like other varieties of diabetes, it is caused by your body being unable to produce or effectively use the insulin it needs during pregnancy. Insulin helps your body to control blood sugar (or blood glucose) levels — not having enough insulin can lead to high blood sugar levels.
Unlike other types of diabetes, gestational diabetes is nearly always temporary and will resolve itself once your baby is born. It does mean that your risk of getting diabetes in the future is higher so it is a good time to learn about the lifestyle changes which are useful to maintain after delivery to prevent diabetes for your longer-term health.
Gestational diabetes can start at any point during a pregnancy, but it is most common during the second and third trimesters (12 weeks of pregnancy onwards). It is for this reason that routine diabetes screening, which is offered to women who meet certain criteria that put them at higher risk of developing diabetes, usually takes place when you are between 24 and 28 weeks pregnant.
It’s rare for gestational diabetes to cause symptoms. However, some women may develop symptoms if their blood sugar levels get too high. These symptoms include:
- increased thirst
- needing to urinate more often than usual
- tiredness
- dry mouth
- blurred eyesight
- genital itching/thrush
If you are worried about any of these symptoms, speak to your midwife or doctor.
What causes gestational diabetes?
It’s not known exactly why some women develop gestational diabetes and others don’t, but there are some risk factors which can make it more likely. These include:
- being overweight/obese with a body mass index (BMI) of 30 or over
- experiencing gestational diabetes in a previous pregnancy
- having had a baby weighing 4.5kg/10lb or more
- having a parent or sibling with diabetes
- having previously had weight loss surgery
- being of South Asian, African-Caribbean or Middle Eastern descent
If you fall into any of the above risk categories, you should be offered routine screening for gestational diabetes.
Complications of gestational diabetes
While most women who experience gestational diabetes will go on to have normal pregnancies and give birth to healthy babies, there is a small number who will experience complications associated with their persistently high blood sugar levels.
These include, but aren’t limited to:
- polyhydramnios: a condition that causes excess amniotic fluid in the womb, which can lead to complications for the baby
- pre-eclampsia: a condition that causes high blood pressure and can lead to pregnancy complications
- your baby growing larger than usual, which could escalate the need for a and increase the risk of complications during labour
- your baby suffering from jaundice (yellowed skin and eyes) at birth
- your baby having very low blood sugar
- higher chance of needing a c-section or experiencing premature birth (birth before the 37th week of pregnancy)
- an increased risk of developing diabetes in the future
- loss of your baby (stillbirth) although this is a very rare complication
For this reason, it’s important to take steps to avoid gestational diabetes.
How to avoid gestational diabetes
Although there is no guarantee that you can prevent gestational diabetes, there are things that you can do to reduce your risk of developing the condition.
Keep active
Exercise may feel like the last thing you want to do when you are pregnant, but keeping active is important. Regular physical activity will help you to manage your weight, stay strong and supple, keep your energy levels up and be in the best shape possible for birth and becoming a mum.
You don’t need to do regimented exercises. Keeping active can be as simple as doing things like:
- taking the stairs rather than the escalators
- walking instead of driving or taking public transport
- going swimming (which is low impact so great during pregnancy)
- walking your dog, or borrowing a friend’s
There are some exercise classes that are specially designed for pregnant women which may interest you, including pregnancy yoga — a fantastic way of lowering your blood pressure, easing your stress and anxiety, helping you to sleep, reducing back pain and helping you to be as strong and flexible as possible.
All of these things can help you to be better prepared for birth and the days and weeks after your baby is born.
Eat a healthy, balanced diet
You may be eating for two (or more), but what you eat during your pregnancy is very important.
A balanced, healthy diet will help ensure that both you and your unborn baby get the perfect blend of nutrients you need. This includes the correct nutrition for foetal development, and to give you the energy to get through your pregnancy as easily as possible.
Ideally, you should follow a diet that is high in fibre and protein, and low in fat, sugar and processed foods. Your doctor or midwife will be able to guide you further.
Start your pregnancy at a healthy weight
While not every pregnancy can be planned in advance, research suggests that women who are already a healthy weight when they become pregnant are generally less likely to develop gestational diabetes.
If you are thinking about starting a family in the future, making sure that you are a healthy weight could help reduce your risk of many types of pregnancy complications, including gestational diabetes.
Some weight gain during pregnancy is inevitable. Most pregnant women will put on between 10kg/22lb and 12.5kg/28lb, but this can vary considerably. Much of this extra weight is your baby, the placenta and amniotic fluid, but some will also be fat that your body is storing ready to make breast milk after the birth.
Your prenatal care team will keep a close eye on how much weight you gain during your pregnancy, which could also be affected by how many babies you are carrying, how old you are and how easily you normally gain weight. If you aren’t gaining enough weight, or you are bordering on gaining too much weight too quickly, your prenatal care team will offer the necessary advice. They often encourage you to maintain a weight neutral pregnancy.
Preventing diabetes after pregnancy
In most cases, the blood sugar levels of someone with gestational diabetes will return to normal after their baby is born. However, some women will go on to develop type 2 diabetes.
It’s important to continue to exercise and follow a healthy, balanced diet after pregnancy as this could reduce the likelihood that you develop type 2 diabetes.
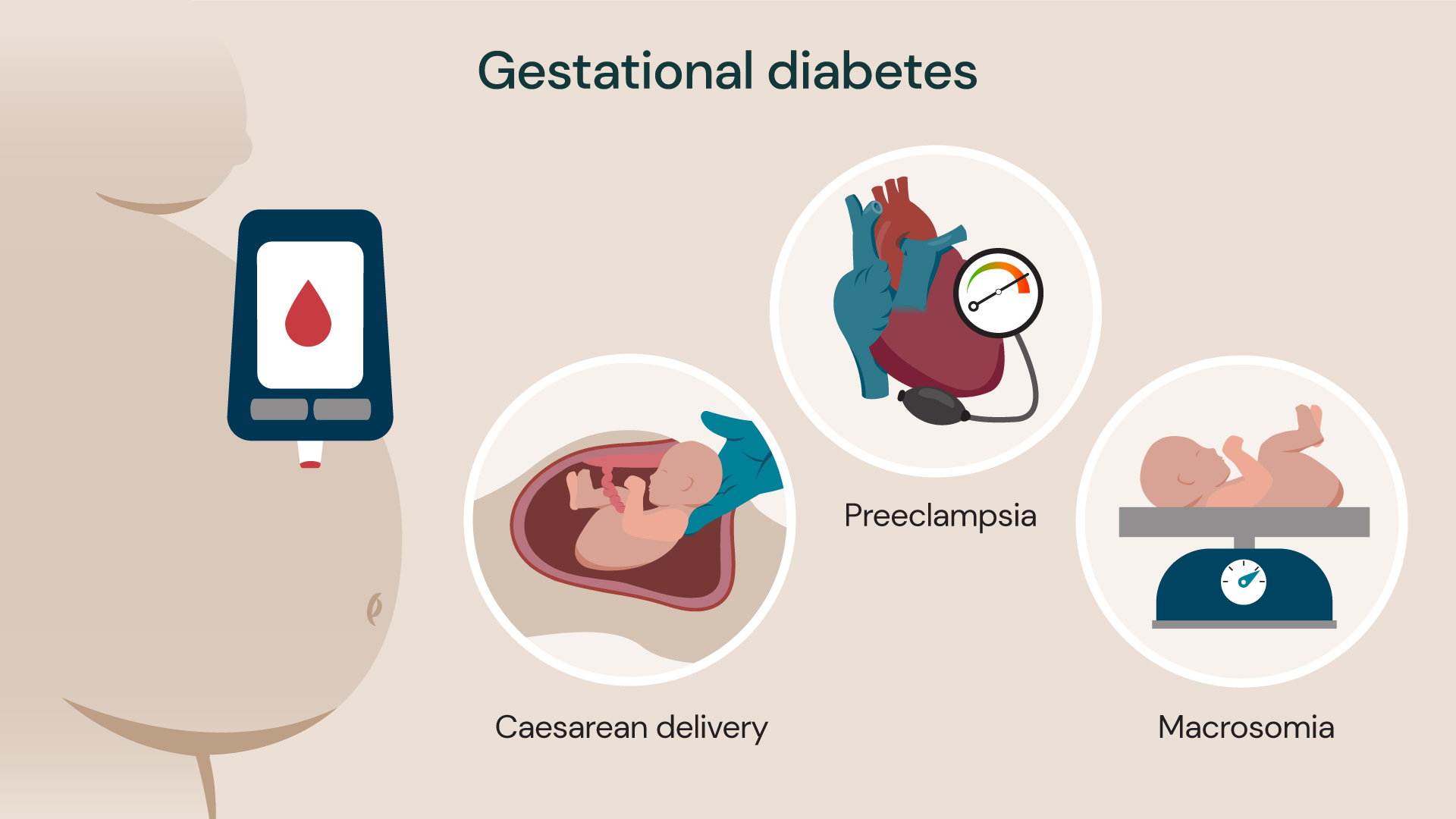
Gestational diabetes can cause issues such as preeclampsia (high blood pressure during pregnancy), caesarean delivery and macrosomia (baby born heavier than average).
How to avoid gestational diabetes
Although there is no guarantee that you can prevent gestational diabetes, there are things that you can do to reduce your risk of developing the condition.
Keep active
Exercise may feel like the last thing you want to do when you are pregnant, but keeping active is important. Regular physical activity will help you to manage your weight, stay strong and supple, keep your energy levels up and be in the best shape possible for birth and becoming a mum.
You don’t need to do regimented exercises. Keeping active can be as simple as doing things like:
- taking the stairs rather than the escalators
- walking instead of driving or taking public transport
- going swimming (which is low impact so great during pregnancy)
- walking your dog, or borrowing a friend’s
There are some exercise classes that are specially designed for pregnant women which may interest you, including pregnancy yoga — a fantastic way of lowering your blood pressure, easing your stress and anxiety, helping you to sleep, reducing back pain and helping you to be as strong and flexible as possible.
All of these things can help you to be better prepared for birth and the days and weeks after your baby is born.
Eat a healthy, balanced diet
You may be eating for two (or more), but what you eat during your pregnancy is very important.
A balanced, healthy diet will help ensure that both you and your unborn baby get the perfect blend of nutrients you need. This includes the correct nutrition for foetal development, and to give you the energy to get through your pregnancy as easily as possible.
Ideally, you should follow a diet that is high in fibre and protein, and low in fat, sugar and processed foods. Your doctor or midwife will be able to guide you further.
Start your pregnancy at a healthy weight
While not every pregnancy can be planned in advance, research suggests that women who are already a healthy weight when they become pregnant are generally less likely to develop gestational diabetes.
If you are thinking about starting a family in the future, making sure that you are a healthy weight could help reduce your risk of many types of pregnancy complications, including gestational diabetes.
Some weight gain during pregnancy is inevitable. Most pregnant women will put on between 10kg/22lb and 12.5kg/28lb, but this can vary considerably. Much of this extra weight is your baby, the placenta and amniotic fluid, but some will also be fat that your body is storing ready to make breast milk after the birth.
Your prenatal care team will keep a close eye on how much weight you gain during your pregnancy, which could also be affected by how many babies you are carrying, how old you are and how easily you normally gain weight. If you aren’t gaining enough weight, or you are bordering on gaining too much weight too quickly, your prenatal care team will offer the necessary advice. They often encourage you to maintain a weight neutral pregnancy.
Preventing diabetes after pregnancy
In most cases, the blood sugar levels of someone with gestational diabetes will return to normal after their baby is born. However, some women will go on to develop type 2 diabetes.
It’s important to continue to exercise and follow a healthy, balanced diet after pregnancy as this could reduce the likelihood that you develop type 2 diabetes.
Related services
-
Gestational diabetes
It’s common to develop diabetes during pregnancy, this is known as gestational diabetes and is usually only temporary.
-
Pre-eclampsia
Pre-eclampsia is a condition that can occur in pregnancy. Find out more.
-
Caesarean section (C-section)
A caesarean section, also known as a C-section, is a birth option for delivering your baby.
