Innovations in fetal monitoring for better cardiac outcomes
About 1% of babies born worldwide have congenital heart disease, one of the most common birth defects, which can cause serious symptoms immediately after birth if undetected during pregnancy. Using pioneering technologies, our consultant fetal cardiologists have developed a world-leading imaging programme to enhance prenatal diagnosis of congenital heart disease.
Fetal diagnosis for better post-birth outcomes
In the UK, the Fetal Anomaly Screen Program (FASP) recommends that every pregnant woman have an ultrasound scan at 18 to 20 weeks. This scan helps to detect major structural problems in all organs of the fetus, including the heart.
“Many women don’t find out their baby has a heart problem until after they are born. It is important to precisely diagnose the type of congenital heart disease in the unborn baby during pregnancy. If the infant requires intervention soon after delivery, we can prepare for surgery and achieve the best outcomes,” – explains Dr Owen Miller, consultant in paediatric and fetal cardiology.
Artificial intelligence to identify cardiac anomalies
To improve detection of congenital heart disease during routine scans, our consultant fetal cardiologists at Evelina London and at our university academic partner Kings College London have developed a “machine learning” approach with the goal of improving both the accuracy and efficiency of these scans.
By processing thousands of ultrasound images through a computer network multiple times, the algorithm gets better each time at telling any difference between two images. When the network automatically identifies a suspected anomaly, our sonographers can review the fetus in further detail for an accurate diagnosis.
“We have trained the network to identify the cardiac chambers and alert us to incongruities in the images that we upload,” – explains Dr Thomas Day, paediatric and fetal cardiologist at Evelina London.
While the technology does not eradicate the need for human review,
“using artificial intelligence has allowed us to perform an anomaly scan seven minutes quicker than a standard, manual scan,” adds Dr Day.
3D MRI technology to enhance expert-level diagnosis
In children with congenital heart disease, cardiac MRI is a safe and well-established method for generating detailed 3D and 4D scans of the heart to enhance expert-level diagnosis. Before birth, however, the constant motion of the baby and the small size of the fetal heart makes this method extremely unreliable, and it is not widely used in clinical practice.
To circumvent these challenges, our consultant team at St Thomas’ Hospital and King’s College London have pioneered novel motion-correction techniques to obtain detailed, high-resolution scans of the fetal heart during pregnancy. These methods use sophisticated artificial intelligence software to re-orientate multiple MRI images into a single three dimensional model and are extremely reliable – meaning we are the only UK centre able to routinely offer 3D MRI for selected patients in addition to fetal ultrasound. Taking the technology one step further, these 3D images can then be converted into a physical representation of the cardiac anatomy, via 3D printing technology.
“Being able to show a parent a 3D version of their unborn baby’s heart is very helpful, and this technology allows us to create images of the heart in a way that the clinicians and patients can better understand,” says Dr Kuberan Pushparajah, consultant paediatric cardiologist. “We are the first centre in the world to do this in a systematic, valid and reproducible way,” he adds.
Our cardiovascular magnetic resonance (CMR) unit is embedded in one of the world’s leading fetal MRI units at King’s College London, which in turn is part of a much wider infrastructure at St Thomas’ Hospital, including ultrasound, fetal medicine and general obstetrics: a set-up which allows for us to care for the whole baby. “All women undergoing fetal cardiac MRI will also have detailed brain and body imaging reported by our expert team of radiologists,” says Dr David Lloyd, consultant paediatric and fetal cardiologist at Evelina London.
“Our team has world-leading experience in advanced prenatal imaging, with a well-established pathway for alerting clinicians quickly to new diagnostic information from these scans,” he continues.
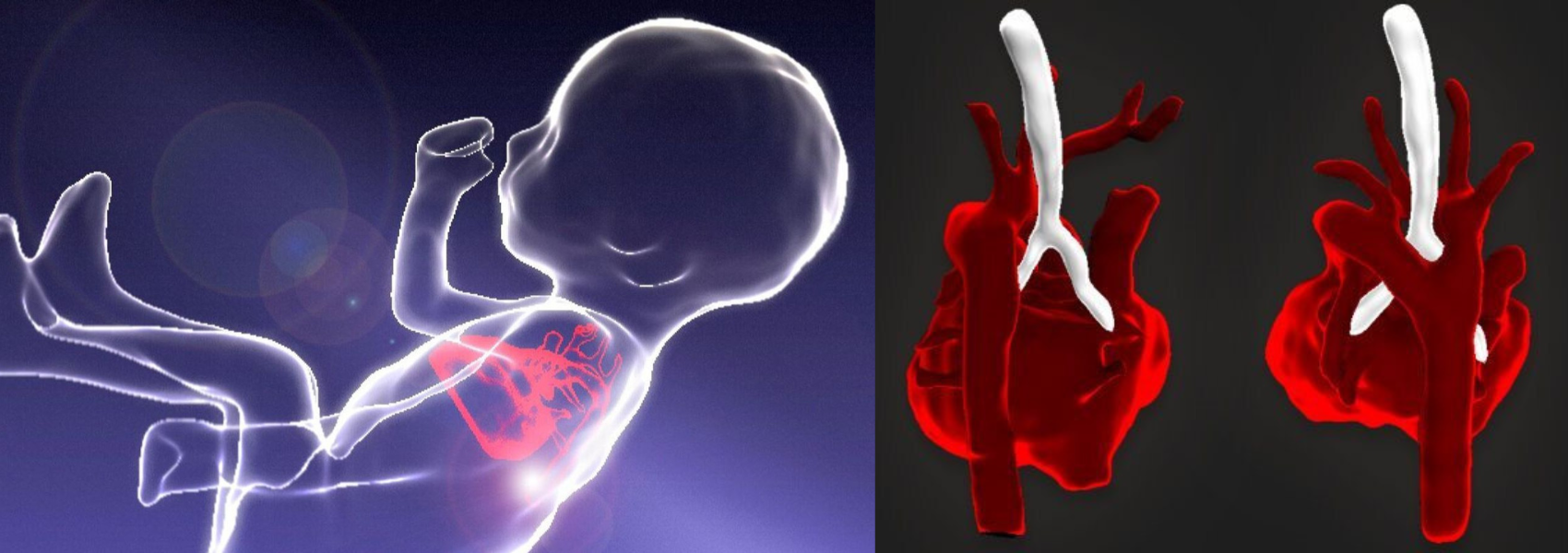
The technique transforms standard images into clear three-dimensional images (left). A 3D MRI scan of a fetal heart (right).

3D-printed models of a fetal heart
Virtual reality for road testing procedures
Furthermore, our consultants have developed a way to translate the 3D images of a fetal heart into a virtual reality (VR) environment. Equipped with a VR headset and handset controls, the technology allows our cardiologists and surgeons to become immersed into the imaging as if they are viewing a real 3D beating heart.
We can then share these 3D images within our multi-disciplinary team as it aids with decision-making, improves understanding of the pathology and we can road test procedures using virtual images. For example, we have put physical and virtual stents into the images to see how they work.
Professor John Simpson, professor of paediatric and fetal cardiology comments: “This is cutting-edge technology. Instead of just looking at the static vessels around the heart, we can actually see the pumping changes in the heart. This is something that could give us a huge amount of additional, dynamic information.”
For more information on our fetal cardiology services, visit our children’s cardiology page or please contact our team.
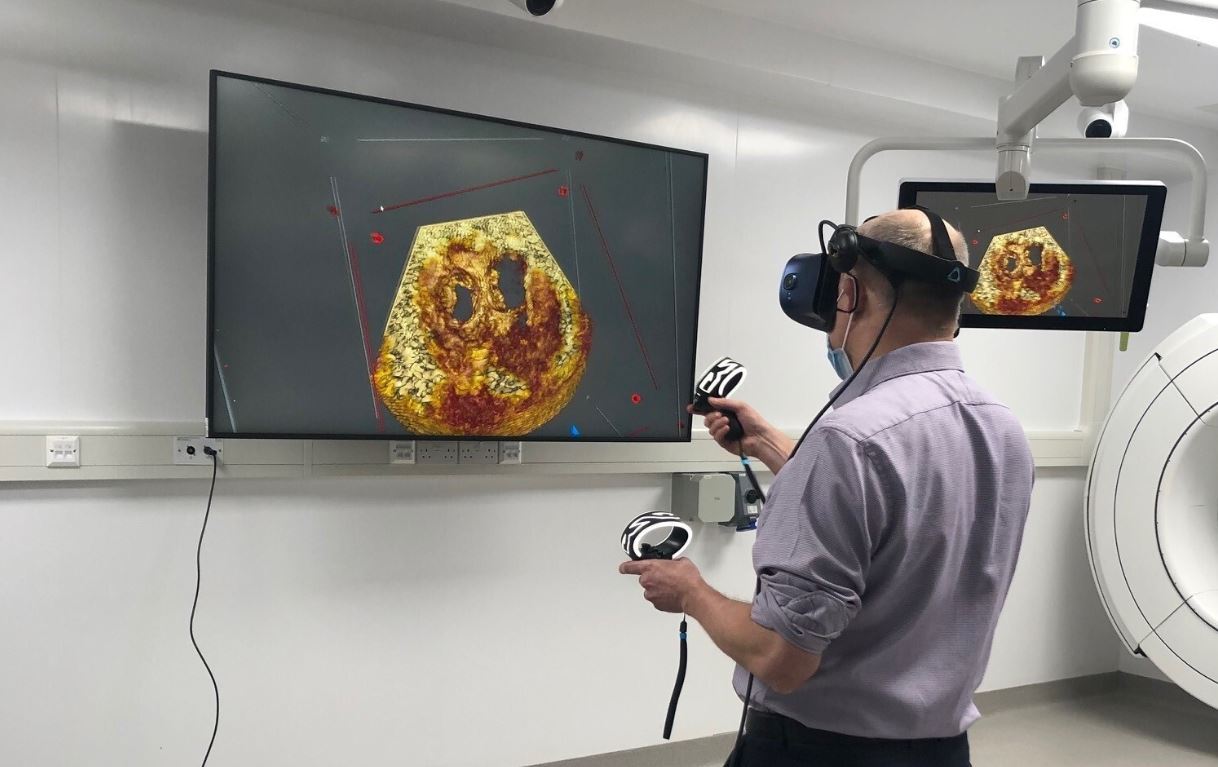
Prof John Simpson using VR technology to view images of the heart
Related content
-
Antenatal tests
As part of our leading private maternity service we offer a range of blood tests, swabs and screenings to support you during your pregnancy.
-
Cardiology
Our specialists are continuously innovating in minimally invasive cardiology procedures and improving care delivery.
-
Fetal cardiology
As one of the largest fetal cardiology units in Europe we manage heart problems in babies before birth.


