Many different health conditions can affect you while pregnant; managing them early on is essential. One condition that can develop during pregnancy is pre-eclampsia.
Early diagnosis of pre-eclampsia is vital for you and your baby’s health and a central aspect of your antenatal care. That’s why our team of specialist obstetricians provide expert maternity care, accurately diagnosing your condition and monitoring you throughout pregnancy.
What is pre-eclampsia?
Pre-eclampsia occurs after the first 20 weeks pregnancy, but you can even develop it after giving birth.
Pre-eclampsia causes high blood pressure and reduces the function of some of your organs, such as your kidneys. Changes to your kidney function can lead to doctors finding proteins in your urine, a sign that you may have pre-eclampsia.
With pre-eclampsia, the placenta does not get enough blood from your body. This disturbs the blood flow between you and your baby putting them at risk of poor growth. Because of these potential complications, doctors may recommend growth scans of your baby and in some cases early delivery of your baby.
If left untreated, pre-eclampsia can be life-threatening to you and your baby.
How common is pre-eclampsia?
Pre-eclampsia is not a common condition but occurs in up to 6% of pregnancies in the UK however, severe pre-eclampsia is rarer, occurring in 1-2% of pregnancies.
Based on certain risk factors, some women have a higher chance of developing pre-eclampsia, for example if you already have high blood pressure your chances of developing the complication increases.
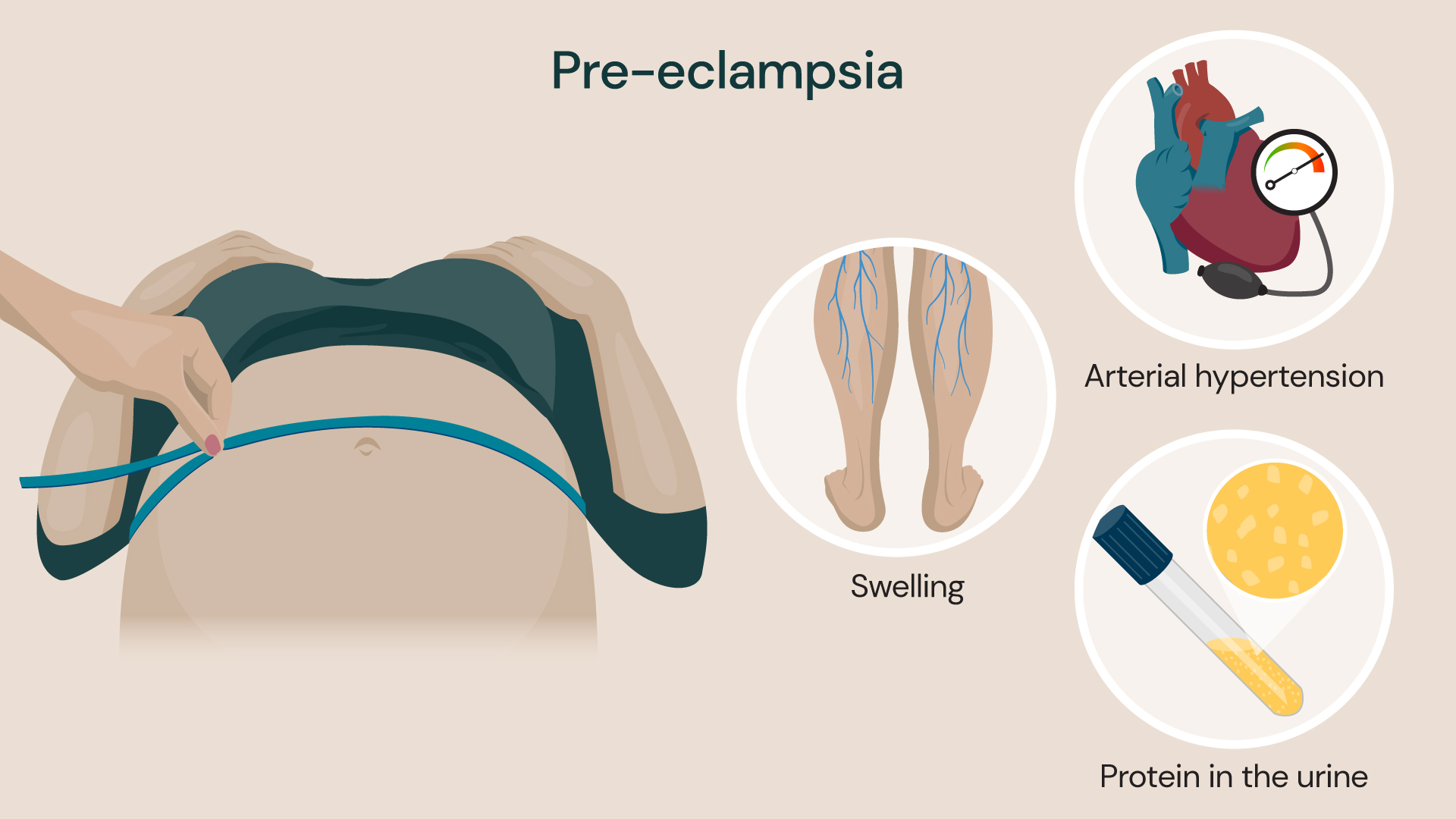
Early signs of pre-eclampsia include high blood pressure, protein in your urine (proteinuria), swelling in your legs, face or hands
Pre-eclampsia symptoms
Most of the symptoms of pre-eclampsia are mild, but careful assessment of your pregnancy by our obstetricians and your midwife can reduce the risk of complications.
Early signs of pre-eclampsia include:
- high blood pressure
- protein in your urine (proteinuria)
You probably won’t notice these signs, but your consultant will pick them up during your antenatal appointments. Having high blood pressure on its own does not mean you have pre-eclampsia. However, if you have this along with protein in your urine, it could be a sign you do.
You can experience other symptoms when you have pre-eclampsia, but these usually only occur when your condition worsens. These can include:
- headaches that don’t go away
- nausea
- dizziness
- swelling in your legs, face or hands
- changes to your vision, such as blurriness
- abdominal pain
- diarrhoea
- sudden weight gain
What causes pre-eclampsia?
The exact cause of pre-eclampsia is not fully understood. However, experts think it’s caused by a problem with the blood vessels in your placenta.
Your placenta links your blood supply to your baby, and supplies food and oxygen to them. It needs a constant supply of blood to support your baby’s needs, but if you have pre-eclampsia, your placenta cannot get this due to reduced blood flow.
It is believed this restricted blood flow is caused by the placenta not developing correctly during the first half of your pregnancy. At around 20 weeks of pregnancy the blood vessels in your placenta become wider. Sometimes, they may not become wide enough — restricting blood flow.
Pre-eclampsia risk factors
Some women can be more at risk of developing pre-eclampsia than others. Factors that can put you at a higher risk of pre-eclampsia include:
- pre-existing medical conditions such as diabetes, high blood pressure, lupus and kidney disease
- previously having pre-eclampsia
Other risk factors that can slightly elevate your risk include:
- a family history of the condition
- you are over 40 years old
- you were obese at the start of your pregnancy (this means having a body mass index (BMI) of over 35
- you are pregnant with multiple babies
- it’s your first pregnancy
- it’s been 10 years since your last pregnancy
Diagnosing pre-eclampsia
During your antenatal appointments, the doctor or midwife will check your blood pressure regularly. They will request a sample of your urine and check for protein. Sometimes, a blood test is carried out to measure levels of a protein called placental growth factor (PlGF). If your PlGF levels are high, you most likely do not have pre-eclampsia. Low levels can indicate pre-eclampsia, but further testing is needed to confirm.
If your GP diagnoses you with pre-eclampsia, our specialists are on hand to help manage your care throughout your pregnancy so you can undergo further tests and monitoring.
Pre-eclampsia treatment
The only cure for pre-eclampsia is delivery of your baby. After a pre-eclampsia diagnosis, we will monitor you very carefully until delivery. If your condition is mild, you should be able to go home and only attend regular check-up appointments. If the condition is moderate or severe, you can be admitted to the hospital and monitored for some time or could have your baby delivered.
When you are in the hospital, you will:
- have your blood pressure monitored regularly
- have regular urine samples taken to measure your protein levels
- undergo different blood tests to check your kidney and liver function
- get ultrasound scans to check your baby’s growth, the blood flow to the placenta and amniotic fluid levels
- have your baby’s heart rate monitored through cardiotocography to ensure they aren’t distressed
Several treatments are available to manage the symptoms of pre-eclampsia. For example, we may give you medication for your high blood pressure to reduce the likelihood of severe complications. Your consultant will create a treatment plan specific to your condition after considering your history and diagnosis.
We recommend delivery of your baby during your 37th or 38th week of pregnancy when you have pre-eclampsia. You may need to have your labour induced or have a caesarean section. If you have severe pre-eclampsia, you may require an earlier delivery.
Pre-eclampsia complications
Complications associated with pre-eclampsia are rare but can occur if your condition is not diagnosed and monitored.
One potential complication of pre-eclampsia is eclampsia (fits). During an eclamptic fit your muscles contract involuntarily for up to a minute. You can lose consciousness and wet yourself. Most fits are harmless, but there is a small risk of brain damage or a permanent disability if the fit is exceptionally severe. In severe pre-eclampsia you may be prescribed magnesium sulphate to prevent eclamptic fits from occurring.
HELLP syndrome is a liver and blood clotting disorder that can develop with pre-eclampsia. This rare condition is most likely to develop after your baby’s birth. However, it can develop at any time after 20 weeks. The condition causes red blood cells in your blood to break down, causing complications with your liver and high blood pressure.
HELLP stands for:
- H – haemolysis
- EL – elevated liver enzymes (proteins)
- LP – low platelet count
Experts consider HELLP more dangerous than pre-eclampsia; the only way to cure it is by delivering your baby.
Other complications affecting you can include:
- stroke
- organ problems such as kidney and liver failure
- blood clotting disorders
After you give birth, your condition should improve within a few days. However, complications can still occur after delivery, so you must stay in the hospital for monitoring. You will undergo blood pressure checks and we will monitor your baby. You may still need to take your blood pressure medication for a few weeks after delivery.
Complications affecting your baby
If you have pre-eclampsia, your baby may grow more slowly in the womb. Slow growth is because the condition restricts the nutrients and oxygen passed to your baby through your placenta. If we must deliver your baby early, it may lead to problems such as breathing difficulties (neonatal respiratory distress syndrome).
Should your baby develop this condition, they will need to stay in neonatal intensive care for monitoring and treatment.
Locations
Westminster Maternity Suite is home to our private maternity services and is available in the following locations:
Discover our maternity experts
Meet our team of leading obstetricians. From pregnancy scans to advanced fetal interventions, our specialists are here to provide you with personalised care.
