Cardiomyopathy refers to a group of inherited diseases impacting the heart muscle. These conditions can affect people of all ages and are a major cause of morbidity and mortality in younger ages, where other cardiac conditions are uncommon. Cardiomyopathies can run in families, affecting several members of a family.
Hypertrophic cardiomyopathy — or HCM for short — is the most common, affecting around 1 in every 500 people in the UK.
What is hypertrophic cardiomyopathy?
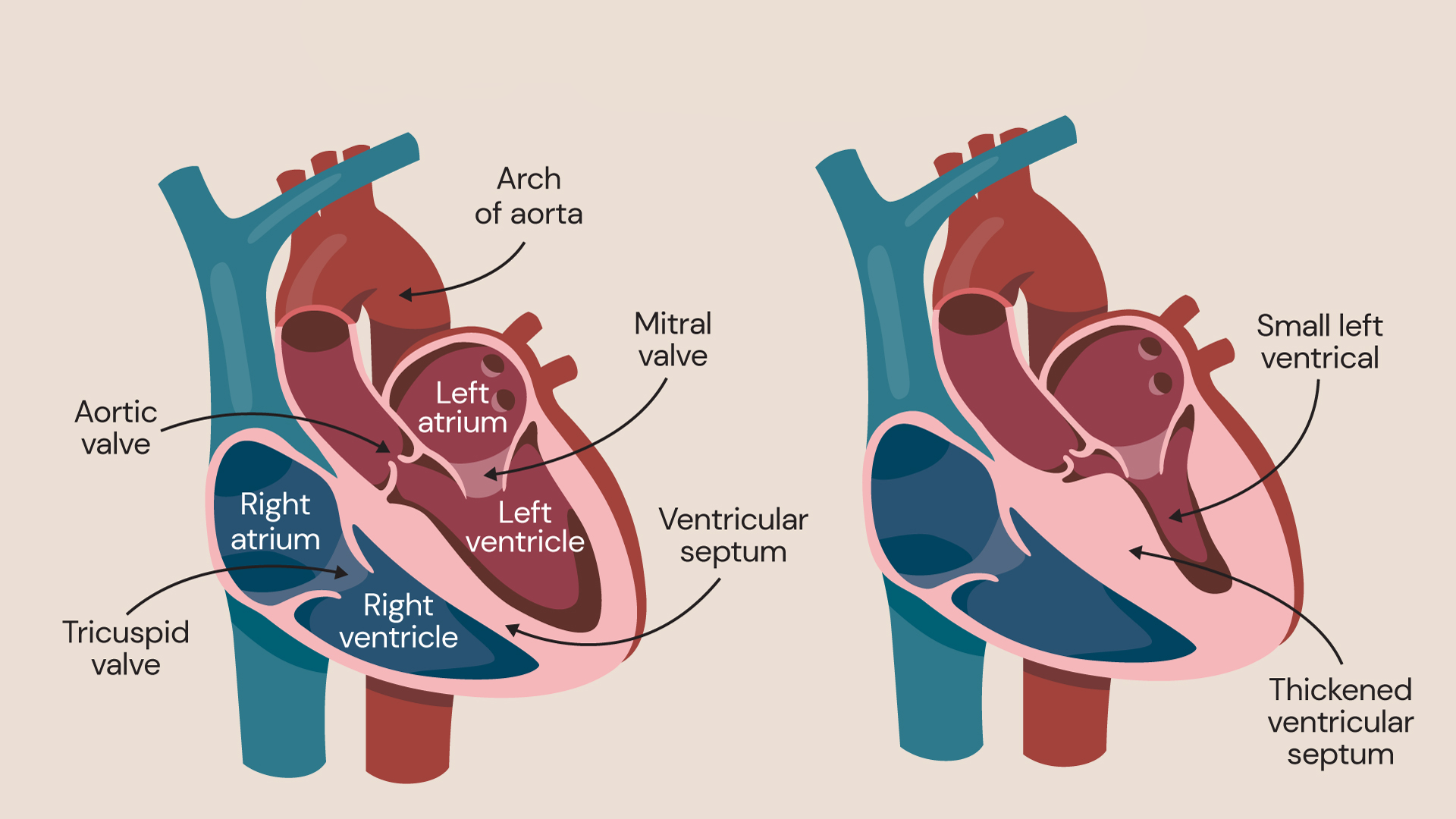
Cardiomyopathy is characterised by a thickening of the heart muscles which can lead to reduced blood capacity and flow.
Hypertrophic cardiomyopathy is characterised by thickening of the heart muscle. Because the walls of the heart chambers thicken, the chambers can’t hold as much blood. Sometimes, the flow of blood through the heart may also be obstructed.
As an inherited condition it is caused by an abnormal genetic variant (a ‘spelling mistake’ in the DNA) in one or more genes and is passed down from parents to children. If your parents have hypertrophic cardiomyopathy, there is a 50% chance you have it too. Some patients have hypertrophic cardiomyopathy due to a new genetic variant which was not present in their parents and can therefore not be present in their siblings. However, it can still be inherited to their children.
Hypertrophic cardiomyopathy affects patients’ lives to a variable degree.
Types of hypertrophic cardiomyopathy
There are two types of hypertrophic cardiomyopathy, known as obstructive and non-obstructive. Both relate to an unusually thick heart muscle, but they also have some key differences.
Nonobstructive hypertrophic cardiomyopathy
In non-obstructive hypertrophic cardiomyopathy, the left ventricle may be thickened enough to become stiff, meaning it needs to work harder than usual to receive the blood from the body and to maintain a good circulation. However, there isn’t any significant blockage affecting blood flow.
This can result in symptoms, depending on how thick your heart muscle is or how stiff it has become.
Obstructive hypertrophic cardiomyopathy
Obstructive hypertrophic cardiomyopathy is named because the thickened heart muscle obstructs the flow of blood leaving the lower left chamber of the heart (the left ventricle).
The mitral valve, which links the upper left chamber (left atrium) with the left ventricle, may also be affected and moves near to or touches on the thickened muscle, which can cause problems with the direction of the flow of blood through the heart.
These changes to the heart create what is known as left ventricular outflow tract obstruction (LVOTO). Around 75% of people with hypertrophic cardiomyopathy have LVOTO, which causes debilitating symptoms and can impact daily life.
Both non-obstructive and obstructive hypertrophic cardiomyopathy can be associated with the risk of sudden cardiac arrest, particularly in young people.
Long-term, hypertrophic cardiomyopathy can lead to enlargement of the left atrium and an increased risk of an irregular and abnormally fast heartbeat — a condition called atrial fibrillation (AF) which may cause symptoms and increase the risk of stroke.
The left ventricular outflow tract obstruction (LVOTO) appears to further increase the risks of sudden death and stroke.
What causes hypertrophic cardiomyopathy?
Hypertrophic cardiomyopathy is nearly always an inherited condition. This means that developing the condition is completely out of your control.
If you have someone in your family with HCM, there is a chance that you will have it too. For this reason, many families that have the condition are offered genetic testing.
Symptoms of hypertrophic cardiomyopathy
There is a broad range of clinical presentations from patients being almost asymptomatic, to patients experiencing debilitating symptoms, mainly during simple physical activity and postural changes. Additionally, some patients prevent their regular symptoms by avoiding certain activities which may indirectly affect their quality of life.
Some patients with obstructive hypertrophic cardiomyopathy may experience symptoms, which may get worse over the time.
Some of the most common symptoms of hypertrophic cardiomyopathy are:
- breathlessness with activity, or after getting up following a period of rest
- fatigue
- light headedness, especially after activity or exercise
- chest pain or tightness (angina)
- fainting or feeling faint during or after exercise
- heart palpitations (where your heart feels like it is beating fast or irregularly)
If you experience any of these and you have not yet been diagnosed with HCM, you should make an appointment with your doctor.
How is hypertrophic cardiomyopathy diagnosed?
Tests for hypertrophic cardiomyopathy include:
- an electrocardiogram, or ECG for short, that records the electrical activity in your heart
- a Holter monitor (a monitor recording the rhythm for one or more days)
- an echocardiogram, which is an ultrasound scan of your heart that looks at its size, structure, and pumping action
- a cardiac MRI (Magnetic Resonance Imaging) scan, which creates highly detailed images of your heart and how it is working
- exercise tests that see you undergo an ECG while you are on a treadmill or exercise bike, and that shows how well your heart works when you are active.
The information from these tests can be used to make a diagnosis of hypertrophic cardiomyopathy and decide which treatment, if any, is required. They also be used to stratify the risk and to decide on prevention.
Additionally, gene testing is offered to see if you carry a faulty gene that could be responsible for HCM, This information can also assist the screening of the family members.
Hypertrophic cardiomyopathy treatment
Currently, there isn’t a specific cure for hypertrophic cardiomyopathy. However, there are treatments that can help keep your symptoms under control and prevent any complications.
Medicines for hypertrophic cardiomyopathy
There are a range of medicines which may be prescribed to help counteract your condition and keep your heart functioning optimally. These work by reducing how hard your heart must work to pump blood around your body, controlling blood flow inside the heart and managing any abnormal heart rhythms. A new medicine has been licenced in the UK very recently and has been added to the previous options. Blood thinning medication is sometimes prescribed to prevent the risk of stroke.
However, as with any medications, there are some side effects that can occur.
ICD (Implantable Cardioverter Defibrillator) surgery
If you are at risk of having an abnormal and life-threatening heart rhythm, you may be recommended to have ICD surgery.
This is where a small device called an implantable cardioverter defibrillator (ICD), is implanted inside your body. It works by detecting abnormal heart rhythms and sending a small electric shock to your heart to return the rhythm to normal.
Pacemaker
Pacemakers are an implantable device that are used to the control your heart rate.
A pacemaker is another type of implantable device that is used to control your heart rate.
Alcohol septal ablation
If you have a significant degree of obstruction in your heart caused by HCM, you may be recommended to have a procedure called alcohol septal ablation (ASA).
ASA is a nonsurgical procedure used to reduce the thickness of the ventricular muscle in the area of the outflow tract.
ASA uses a combination of specialist imaging and the injection of a small amount of ethanol into the small artery that supplies blood to the thickened part of the heart. This causes scarring and shrinking of the wall thickness, which can reduce or even eliminate the blockage.
ASA can only address the muscle thickness and not the other components of the internal anatomy of the heart, and the amount of muscle mass reduction is also limited.
In cases where a significant reduction of the wall thickness would be required, it would mean inducing a large myocardial infarction (a heart attack), which increases the risk of the procedure.
In general, the risk of major complications is about similar to the risks of major complications with surgery — around 1%. But with ASA, patients benefit from a shorter hospital stay and more rapid recovery.
Surgical myectomy
Finally, surgery may be used to remove some of the thickened muscle from the heart.
Surgical myectomy for the management of obstructive hypertrophic cardiomyopathy is a procedure which entails surgical muscle resection to eliminate LVOTO. It is a complex, open surgery.
The surgery is planned carefully with the assistance of specialist imaging — including a transoesophageal echocardiogram (TOE) and cardiac MRI — to assess the LVOTO and the anatomy of the left ventricle and the mitral valve.
During the procedure, the surgeon will reach the inside of the heart, through the aorta and the aortic valve. The inner surface of the heart muscle will then be cut under direct vision in order to relieve the blockage in the areas where it is thickened — between 3g and 15g of muscle may be removed to relieve as much of the blockage as possible.
Reducing the blockage can also help to counteract issues with the flow of blood caused by issues with the mitral valve.
Following uncomplicated surgery, a patient can be discharged from the hospital within seven days. The relief from obstructive symptoms is rapid but the recovery from the operation may take a while.
Lifestyle changes
You may also be advised to make some changes to your lifestyle — for example, you may be recommended to avoid high-intensity exercise or change your job if you have a very physically-demanding role.
There are also some rules around living with HCM and driving commercial vehicles like buses and lorries, so you should speak to your doctor about this, or visit the DVLA website.
Related services
-
Atrial fibrillation
Atrial fibrillation is a heart rhythm disorder where your heart beats irregularly, either too fast or too slow. Learn about how our cardiology specialists can treat it.
-
Arrhythmia (abnormal heart rhythm)
Arrhythmia is an abnormal heart rhythm, where the heart’s normal rhythm is disrupted.
-
Cardiac MRI scan (CMR)
A cardiac magnetic resonance (CMR) scan is non-invasive and shows detailed images of your heart.
-
Diagnostic tests for heart conditions
We offer a range of diagnostic tests at our state-of-the-art facilities.
-
Echocardiogram
An echocardiogram – also known as an echo – is a scan that examines the heart and surrounding blood vessels.
-
Electrocardiogram (ECG)
An electrocardiogram (also known as an ECG) is a test which is used to check your heart’s rhythm and electrical activity.
-
Heart failure
Heart failure occurs when the heart stops being able to pump blood around the body in an efficient way.
-
Left ventricular outflow tract obstruction (LVOTO)
Left ventricular outflow tract obstruction (LVOTO) is a recognised feature of hypertrophic cardiomyopathy.
-
Pacemakers and implantable cardioverter defibrillators (ICDs)
Pacemakers and ICDs are different types of implanted electronic devices that are capable of regulating heart rhythm disturbances.
Locations
Discover our cardiology experts
Meet our team of renowned cardiology specialists. From cardiovascular health assessments to innovative interventions, our experts are committed to delivering personalised care designed just for you.
