Hydroceles are typically found in newborn boys, especially premature babies, and sometimes in younger children. Most of the time, they resolve themselves. However, some cases may need surgical intervention to correct them, if they persist or if they are very large.
As part of our paediatric urology service at Evelina London Children’s Hospital, we can treat hydrocele in children of all ages. Our expert team will guide you and your child through the entire process.
What is a hydrocele?
A hydrocele is a swelling in the scrotum and occurs when fluid collects in the thin sac surrounding your child’s testicles. Hydroceles in children often go away without medical intervention by the time they reach age one. However, in some children it can persist and at times older children can also develop a hydrocele.
Hydroceles are primarily painless, but you should still seek the advice of a doctor if your child’s scrotum looks swollen as there could be other causes for it.
Types of hydroceles
The two types of hydroceles are communicating hydroceles and non-communicating hydroceles. The main difference between them is whether they connect to the abdomen.
Communicating hydroceles have a two-way connection between the scrotum and abdomen so fluid can pass between both areas causing fluctuation in size.
In non-communicating hydroceles there is only a one way connection so the fluid remains in the scrotum.
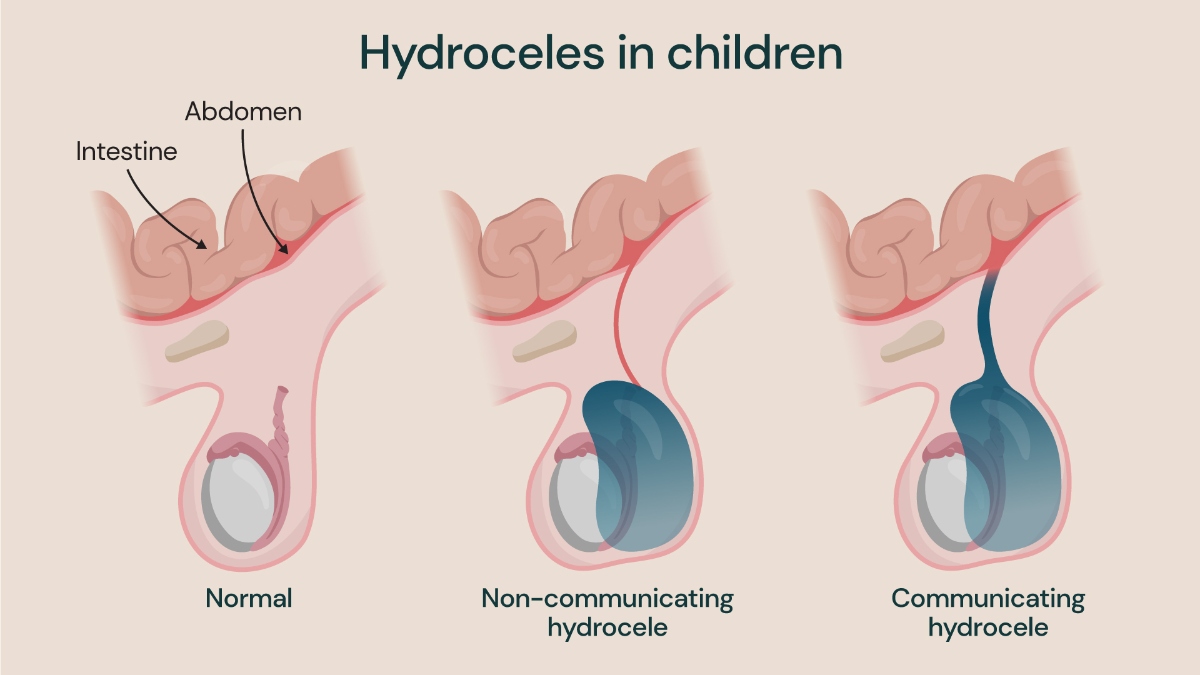
Three diagrams showing a normal scrotum, a non-communicating hydrocele and communicating hydrocele.
What causes a hydrocele?
The most common cause of hydroceles in newborns happens during fetal development. During the fetal development, the testicles move from the abdomen to the scrotum. A sac-like lining from the abdominal cavity is also brought down along with the testes. Usually, the sac closes before birth and the body absorbs the fluid – preventing it from entering the scrotum. However, when it does not, it causes a communicating hydrocele.
Non-communicating hydroceles occur when this connection is partially closed, causing a one-way valve mechanism.
Hydrocele symptoms
Generally, the only symptom of a hydrocele is a painless swelling in either one or both of the testicles. However, it can make your child’s scrotum feel heavier than average and pain can occur if the swelling continues to increase or get infected.
You may notice that their scrotum is more swollen at night and less first thing in the morning. At times the swelling can be aggravated by viral infections like the common cold.
How to prevent hydrocele
As most hydroceles are present at birth, preventing them is impossible. Nevertheless, premature babies are more likely to be born with them.
Sometimes older children can develop hydrocele secondary to following conditions:
- injury of the scrotum
- scrotal inflammation
- infections
- tumours
The secondary hydroceles are far less common in children, but it is essential to diagnose and treat them in a timely manner.
Hydroceles are not considered a dangerous condition in general, however, they can be linked to underlying health conditions, such as an inguinal hernia.
How is a hydrocele diagnosed?
A physical examination of your child’s scrotum and the surrounding area by one of our specialists will help diagnose a hydrocele. The consultant will apply pressure to their groin and ask them to cough to see if the swelling changes or if they experience any pain. Sometimes, a light is shone through the scrotum to see the fluid.
Frequently, a physical examination is all a doctor needs to diagnose hydroceles. However, we can perform other tests to confirm this.
These tests include:
- blood tests to check for an infection
- imaging tests such as a pelvic ultrasound to provide a clear picture of the hydrocele and rule out any underlying cause
Hydrocele treatment
Doctors rarely treat hydroceles in babies as they usually resolve themselves. However, it’s important to seek medical advice if you notice any signs of swelling in your child’s scrotum.
Surgery typically is needed for hydroceles that do not go away on their own. The procedure is called a hydrocelectomy or ligation of patent processus vaginalis (PPV). If surgery is necessary, your child will be given general anaesthetic and be asleep throughout the procedure.
The surgeon will generally make an incision in the lower abdomen then disconnect and close the communication between the abdomen and scrotum.
They will then close the incision with self absorbent sutures and apply a bandage/ medical glue, which is waterproof, to protect the area. The entire procedure should take less than one hour.
Risks of a hydrocelectomy
All surgical procedures carry risks, including hydrocelectomy.
The risks of a hydrocelectomy include:
- reactions to the anaesthesia
- infection
- swelling
- bruising
- scarring
- recurrence
- haematoma (masses of clotted blood)
- injury to vas (sperm tube) and testicular blood vessels as they are closely located to the communication channel
However, the risks during a hydrocelectomy are minimal and the procedure has a high success rate.
Recovery after a hydrocelectomy
A hydrocelectomy is a day case surgery that will take place at our Children’s Day Surgery Unit at Evelina London. Your child will be able to go home on the same day.
If they had a large hydrocele removed, their scrotum can appear slightly stretched. This will shrink back to normal within a few weeks.
Showering can be resumed from the next day to help keep the area clean. It is advised to avoid strenuous activity for at least one week after hydrocelectomy.
Everyone’s recovery is different, so healing time can vary. You should help your child follow any aftercare advice their doctor gives to minimise potential risks, such as infection, and to enhance their recovery.
Locations
Hydrocele treatment is available at the following locations:
Discover our children's urology experts
Meet our team of paediatric urologists. From bladder health to advanced kidney interventions, our specialists are here to provide you with personalised care.
