There are many issues that can occur during the course of a pregnancy, including diabetes. Most people have heard of diabetes, but many are unaware that even if they don’t usually have diabetes, it’s possible to develop the condition during pregnancy.
The good news is that it’s nearly always temporary, and with the right care from our specialist maternity team, it’s possible to limit the effects that it has on you and your unborn baby.
What is diabetes?
Diabetes is a very common condition that affects about 6% of the UK population. It occurs when your body is unable to regulate the amount of sugar in your blood, causing your blood glucose (blood sugar) levels to become too high.
When this happens, it’s normal to experience a range of symptoms that can be quite debilitating. In some cases, untreated diabetes can cause severe and even life-threatening complications.
Types of diabetes
There are several different types of diabetes. Around 90% of people with diabetes have type 2 diabetes, while around 8% have type 1. Gestational diabetes affects around one in 20 pregnancies.
Type 1 diabetes
Type 1 diabetes is a lifelong condition that occurs when your body’s immune system attacks and destroys the cells that produce insulin — the hormone that controls your blood glucose levels.
People with type 1 diabetes need to regularly check their blood glucose and take insulin every day to keep their blood glucose levels under control.
Type 2 diabetes
Type 2 diabetes is also characterised by high blood glucose. However, in type 2 diabetes, the body does not produce enough insulin to function properly, or the body’s cells do not react to insulin as they should. This means that your blood glucose levels will keep rising.
Some things can increase your risk of getting type 2 diabetes. Being overweight or inactive, or having a family history of type 2 diabetes are risk factors.
Without treatment, persistently high sugar levels can cause serious damage to parts of your body, including your eyes, heart and feet.
Gestational diabetes
It’s fairly common to develop diabetes during pregnancy, with around 1 in 20 women affected.
This is known as gestational diabetes and is usually only temporary, caused by your body being unable to produce enough insulin to meet your extra needs during pregnancy.
Gestational diabetes can occur at any stage of your pregnancy but is more common in the second or third trimester. It typically disappears after giving birth.
Signs of diabetes in pregnancy
Diabetes during pregnancy rarely causes any symptoms but can be detected during a routine blood test. Screening for diabetes is a normal part of prenatal care, and this is when most women with the condition are diagnosed.
Nevertheless, there are symptoms that can occur, including:
- increased thirst
- needing to urinate more often than usual
- tiredness
- dry mouth
- blurred eyesight
- genital itching/thrush
If you experience any of these symptoms, it’s important to speak to your midwife or consultant.
What causes diabetes in pregnancy?
Anyone can develop diabetes during pregnancy, but there are specific factors which can increase your risk of the condition. These are:
- being over the age of 40
- having a body mass index (BMI) over 30
- having had gestational diabetes in a previous pregnancy
- having previously had a baby weighing 4.5kg/10lb or more at birth
- a parent or sibling with diabetes
- a previous gastric bypass or other weight loss surgery
- being of South Asian, African-Caribbean or Middle Eastern ethnicity
Pregnant women who fall into any of the above risk categories should be offered routine screening for gestational diabetes.
Diabetes in pregnancy risks and complications
It’s important to get checked for diabetes during pregnancy. While most women with gestational diabetes will go on to have perfectly normal, healthy pregnancies and babies, there are some risks associated with the condition.
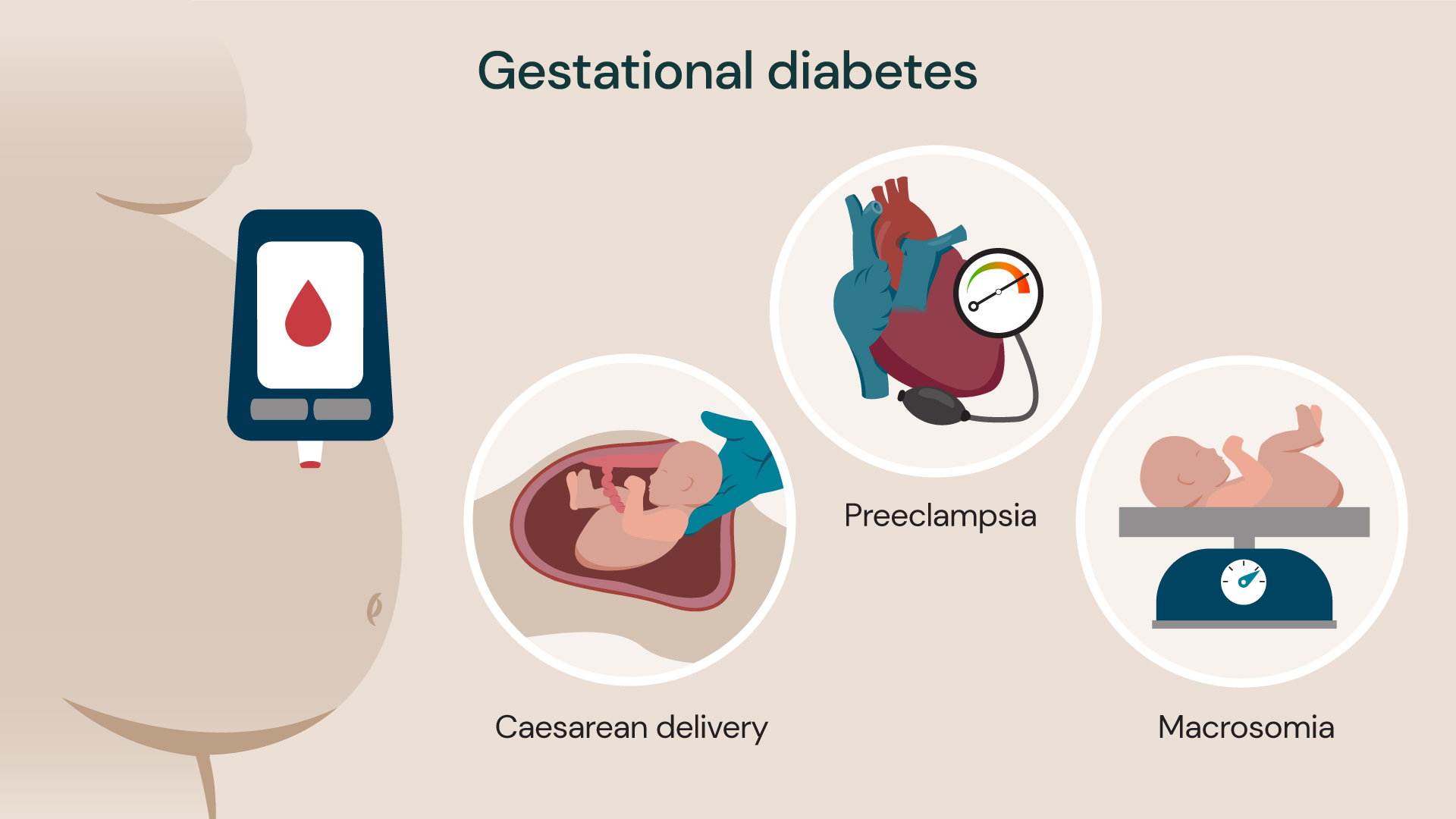
Gestational diabetes can cause issues such as preeclampsia (high blood pressure during pregnancy), caesarean delivery and macrosomia (baby born heavier than average).
Diabetes in pregnancy can cause problems such as:
- pre-eclampsia, a condition that causes high blood pressure and can lead to pregnancy complications
- premature birth (birth before the 37th week of pregnancy)
- your baby growing larger than usual (macrosomia), which could increase the risk of complications during delivery, and the need for a caesarean section
- polyhydramnios, a condition characterised by too much amniotic fluid (the fluid that surrounds the baby in the womb) which can lead to complications
- your baby suffering from jaundice (yellowed skin and eyes) at birth
- your baby has very low blood glucose
- loss of your baby (still birth) although this is a very rare complication
Developing diabetes during pregnancy also puts you at an increased risk of developing type 2 diabetes in the future.
Diagnosing diabetes in pregnancy
Your doctor or midwife will assess your risk of gestational diabetes early on in your pregnancy, usually at around 8 to 12 weeks which is when your first antenatal appointment should take place.
If you are considered to be at high risk (based on the risk factors listed above) you will be offered a screening test, called an oral glucose tolerance test, or OGTT. This test involves three steps:
- You will be given a fasting blood test. This is where you are asked not to eat anything for 8 to 10 hours before your blood is taken but you can continue to drink water.
- You are then given a glucose drink and asked to rest for around 2 hours.
- A second blood test is taken to determine how well your body manages the glucose.
The entire appointment usually takes around 2 hours and is carried out when you are between 24 and 28 weeks pregnant, which is when gestational diabetes is most likely to develop. However, if you’ve had diabetes during pregnancy before, you may be offered the test earlier on when you book your pregnancy.
Treating diabetes in pregnancy
The risks associated with gestational diabetes can be significantly reduced by getting — and keeping — your blood glucose levels under control.
You can do this without medication, such as by changing your diet to include less sugary/sweet and processed food and getting gentle exercises such as swimming, walking and yoga. Just be sure to check with your midwife before starting any new activity.
If your blood glucose levels can’t be properly controlled through diet and exercise alone, you’ll be prescribed medication to help too. This is usually in the form of tablets or injections, but your maternity team will explain what medication you will need to take and how it should be administered.
You may also be advised to deliver your baby before 41 weeks. In some cases, this means being induced (having drugs to put you into labour if it doesn’t happen naturally).
For more information, please read our article on how to avoid gestational diabetes.
Related services
-
Antenatal tests
As part of our leading private maternity service we offer a range of blood tests, swabs and screenings to support you during your pregnancy.
-
Pre-eclampsia
Pre-eclampsia is a condition that can occur in pregnancy. Find out more.
-
Caesarean section (C-section)
A caesarean section, also known as a C-section, is a birth option for delivering your baby.
-
Pregnancy scans
Our comprehensive pregnancy scanning service offers the latest in private ultrasound scans and fetal medicine.
-
Antenatal classes
Our antenatal classes are a great way for expectant parents to prepare for pregnancy, birth and parenthood.
Locations
Westminster Maternity Suite is home to our private maternity services and is available in the following locations:
Discover our maternity experts
Meet our team of leading obstetricians. From pregnancy scans to advanced fetal interventions, our specialists are here to provide you with personalised care.