Coronary heart disease is a serious health problem that affects more than two million people in the UK. Coronary heart disease (or CHD) is also known as ischaemic heart disease.
Coronary heart disease causes chest pain or angina, as well as heart attacks that can result in permanent damage to your heart. Currently, heart and other circulatory diseases kill one in four people in the United Kingdom. However, with early diagnosis and effective treatment, you can protect your heart and prevent further cardiac damage.
What happens in coronary heart disease?
In coronary heart disease, the blood vessels that supply blood to your heart gradually become narrowed by fatty deposits or atheroma. This is often described as ‘furring up’ of the vessels. Fatty plaques build up within the walls of the arteries, narrowing them and restricting the blood flow to your heart muscles in a process known as atherosclerosis.
“Blood provides the oxygen the heart muscles need to function and stay alive. If the vessels are clogged, the muscles can’t get enough oxygen, which causes chest pain or angina. If a piece of the fatty material breaks off, a blood clot may form. This clot can block one of the coronary arteries, cutting off the supply of essential blood and oxygen. Without prompt medical treatment, cells in the heart muscle can die. This is known as a heart attack or myocardial infarction,” explains our consultant cardiologist Dr Georgios Karagiannis.
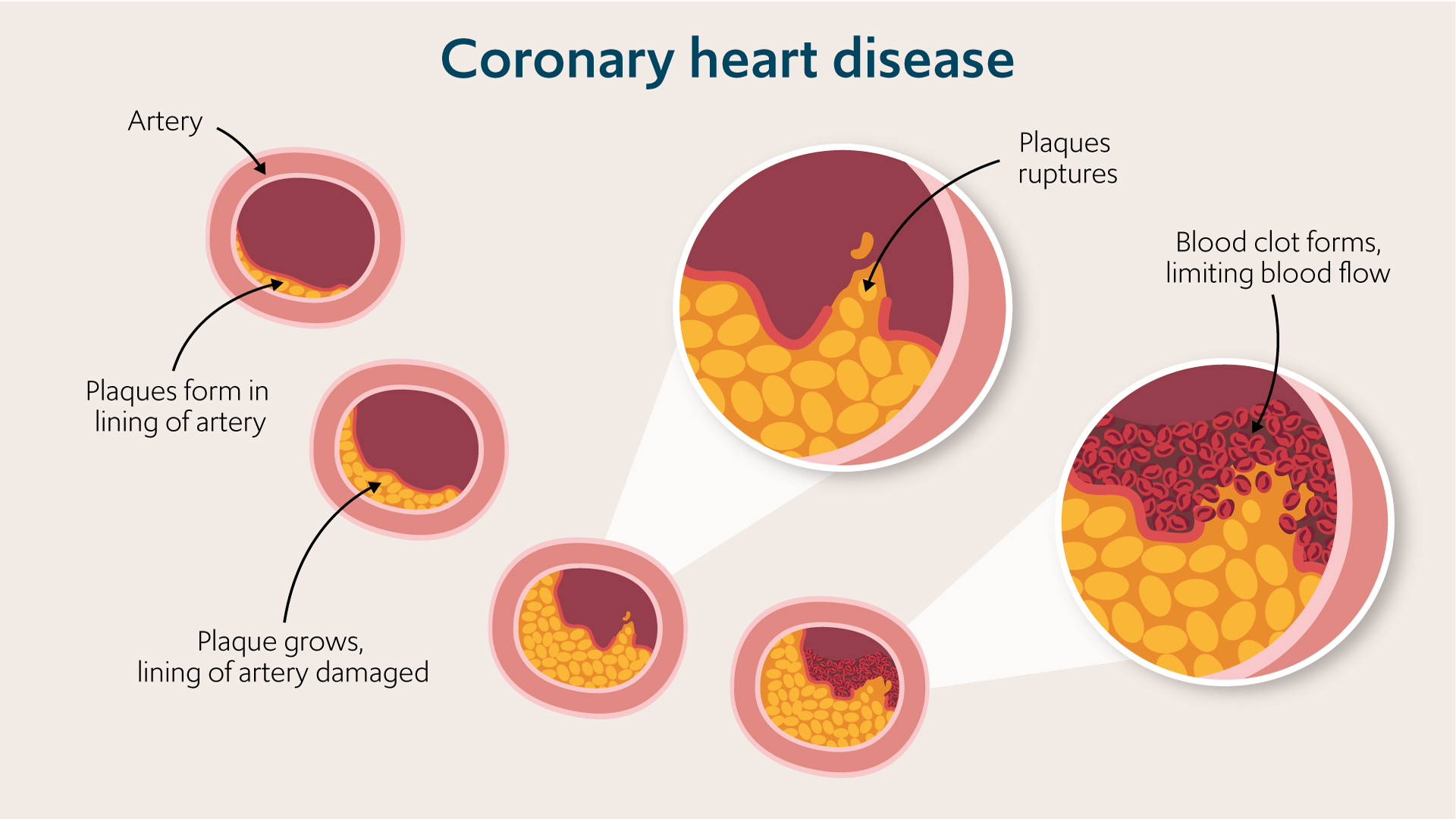
Build up of fatty plaques in the blood vessels causes narrowing and restriction of blood flow.
Symptoms of coronary heart disease
The symptoms of coronary heart disease can differ between people. CHD develops slowly over time, and the symptoms will vary depending on how advanced your coronary heart disease is. There are classic symptoms to look out for; however, some people have no symptoms before having a heart attack.
What are the symptoms of angina?
CHD causes chest pain, known as angina. The symptoms of angina include:
- chest pain that can spread into your arm, jaw, neck or back. The pain can feel like a tightness across the chest or dull and heavy. The pain typically occurs when your heart has to do more work, such as when exercising, exerting yourself or under stress
- shortness of breath
- feeling weak and faint
- nausea
Angina chest pain and discomfort usually stop when you rest for a few minutes. If you experience more severe chest pain, it comes on when you are resting or doesn’t go away; you may need emergency medical care to prevent or treat a heart attack.
What are the symptoms of a heart attack?
A heart attack typically causes chest pain, breathlessness, weakness or feeling faint, sweating and feeling anxious or unwell. However, the symptoms of a heart attack differ between individuals. Some people, especially women, experience milder pain which can be mistaken for indigestion. If you have a combination of symptoms that could indicate a heart attack, act quickly by calling 999. Early treatment can prevent permanent damage to the heart and save your life.
Symptoms include:
- a tight, heavy or crushing chest pain which may spread into your arms, neck, jaw or through to the back. The pain will typically continue when you are at rest, and the pain can come on suddenly, or it may persist over several days
- breathlessness
- cold sweat or clamminess
- feeling unwell and weak
- nausea and sickness
Less commonly, you may experience:
- severe and overwhelming anxiety
- sudden coughing and shortness of breath as a result of fluid accumulating in your lungs
What are the symptoms of heart failure?
Over time, coronary heart disease can damage and weaken your heart, causing heart failure. When your heart is failing it can’t pump effectively, and fluid builds up in your lungs and body. The symptoms of heart failure include:
- breathlessness that is usually worse when lying flat
- swelling or oedema in your feet and ankles. Swelling can also build up in the lower back and genitals, particularly if you have poor mobility
- feeling weak and tired
What are the risk factors for coronary heart disease?
Coronary heart disease is the most common type of heart disease. In the UK, around 7.6 million people are living with heart and circulatory diseases, so anyone could potentially be affected. However, some people are at increased risk of developing CHD. Risk factors include:
- increasing age: CHD is more common in the elderly
- being male: heart disease is more common in men and women after the menopause
- high blood pressure.
- family history of coronary heart disease.
- ethnicity: CHD is more common in people of black African, African Caribbean and South Asian origin
- high cholesterol, particularly increased levels of ‘bad’ or LDL cholesterol
- diabetes
- smoking
- being obese or overweight
- being physical inactive
Can you reduce your risk of developing coronary heart disease?
There are some coronary heart disease risk factors that you can’t control, like your ethnicity and genetic heritage. However, many lifestyle changes can reduce your risk of developing CHD or prevent it from getting worse. Lifestyle changes that can protect your heart include:
- stopping smoking
- exercising regularly
- losing weight to achieve a healthy BMI if you are overweight or obese
- eating a healthy, balanced diet
- taking medication to control any medical conditions like hypertension or diabetes
Coronary artery disease treatment
Doctors can’t cure coronary artery disease, but treatment can increase the blood flow through your coronary arteries, reduce chest pain and prevent heart damage.
Coronary artery disease treatment includes support to reduce any risk factors, effective treatment of diseases such as hypertension and diabetes and treatment to improve the blood flow to the heart muscles.
“The right treatment for your coronary heart disease will depend on your heart and general health. Treatments include medications, minimally-invasive interventions to open up the coronary arteries, and surgery,” explains Dr Karagiannis.
Coronary heart disease medication
Coronary heart disease medications can treat your symptoms and boost the blood flow to your heart. Your doctor or cardiologist may prescribe one or more types of medicine, which could include:
- Nitrates to open up the blood vessels, improve blood flow through the clogged blood vessels and ease chest pain. Different formulations are available: tablets or aerosol sprays under your tongue act quickly to treat pain. Alternatively, pills or self-adhesive patches release medicine over a period of time to prevent angina attacks
- Antiplatelet drugs such as aspirin to reduce clot formation
- Statins or PCSK9 inhibitors to reduce LDL cholesterol
- ACE inhibitors treat hypertension and relax the blood vessels to increase blood flow
- Calcium channel blockers open up your coronary arteries by relaxing the muscles in their walls; they also reduce your blood pressure
- Beta-blockers treat high blood pressure, slow the heart rate and improve blood flow in the vessels
- Diuretics: Water tablets help get rid of excess fluid, treating heart failure and pulmonary oedema
- Antiarrhythmic medicines can treat any abnormal heart rhythms
- Digoxin is used to treat the abnormal heart rhythm atrial fibrillation
Coronary angioplasty and stenting
“Coronary angioplasty is one of the most common treatments for coronary heart disease. It is a minimally invasive intervention that treats coronary artery blockages and improves blood flow through the vessels,” explains Dr Karagiannis.
Through a vessel in the groin, a specialist inserts and inflates a balloon that stretches open the narrowed artery. Usually, they will then insert a short tube, called a stent, into the artery, which remains in place permanently to keep the vessel open.
You can have an angioplasty as an emergency if a clot suddenly blocks the artery or as a planned treatment.
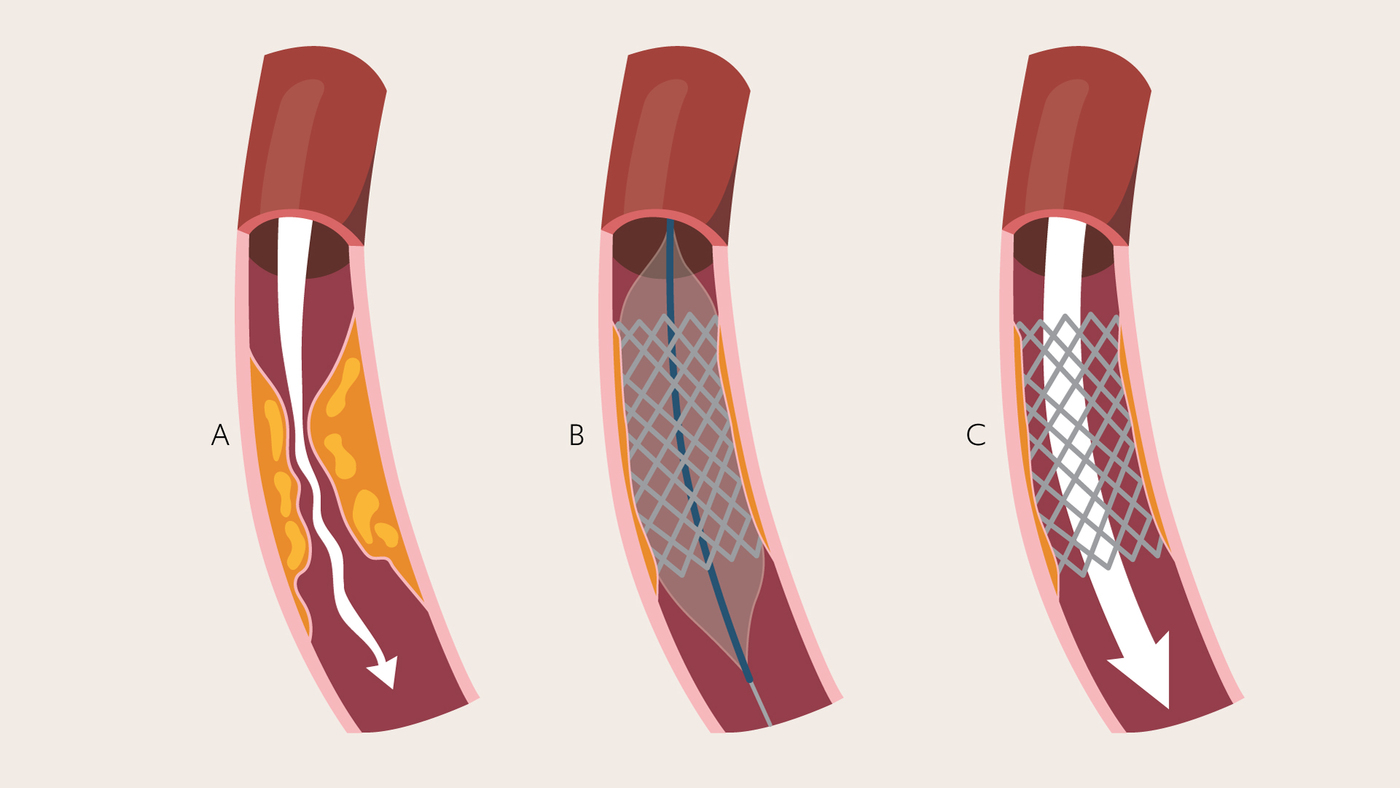
Stents are inserted into the vessels using a catheter via a vessel in the groin.
Coronary artery bypass graft
If your coronary arteries are significantly narrowed, and angioplasty is not possible or has failed, you may benefit from surgery to bypass the blocked blood vessels. In a coronary artery bypass graft or CABG, a cardiothoracic surgeon inserts a new blood vessel into the heart, grafting it to the existing arteries. The new blood vessel bypasses the blocked artery, allowing blood to flow to the heart muscle.

